Two patients with HIV are in remission. How many more will follow them?
And then there were two.
A London man infected with HIV has gone into long-term remission after getting a special stem cell transplant that not only treated his cancer, it sent the virus into remission as well. His recovery, described this week in the journal Nature, marks the second time a patient has cleared HIV from his system with the help of a stem cell transplant.
Will there be more?
Doctors do not see the risky procedure as a way to treat the millions of people who are HIV-positive and at risk of developing AIDS. But it could help researchers design an equally effective treatment that alters a patientâs DNA with pinpoint precision.
The apparent cure of the âLondon patient,â who has not been identified, follows several unsuccessful efforts to replicate the 2008 experience of Timothy Brown, the âBerlin patientâ who underwent treatment for leukemia and gained a robust resistance to HIV in the process. It has raised new hopes that a disease now held in check by costly drugs that must be taken every day could soon be cured with a single infusion of engineered immune cells.
At the dawn of an age in which genetic engineering and immunotherapy promise to become commonplace tools in medicine, the insights gleaned from these two patients could lead to a cure for a disease that has claimed 35 million lives and still kills 940,000 people per year.
âThis is both really exciting and really important,â said Jonah Sacha, an immunologist at Oregon Health and Science University who studies HIV and was not involved in the new research.
âIt really gives a lot of hope to the HIV-cure field,â Sacha said. âBut it also underscores the scale of the task ahead. Itâs huge.â
Across the globe, nearly 37 million people are infected with the human immunodeficiency virus. Some 21 million are taking anti-retroviral drugs daily to suppress their infection.
But drug-resistant strains are surfacing routinely. Thatâs caused worry about the long-term viability of current anti-retroviral medications and added urgency to the search for a way to knock out HIV for good in a single shot.
The London patient had long managed his HIV with anti-retroviral drugs. The bigger health scare came in 2012, when he was diagnosed with advanced Hodgkinâs lymphoma.
After the patient failed treatment with chemotherapy and proved unable to muster the necessary stem cells to provide his own transplant, doctors turned to an international registry to find a suitable stem cell donor. In addition to seeking a close match to the patient, they looked for someone who inherited a particular version of a particular gene from both their mother and their father.
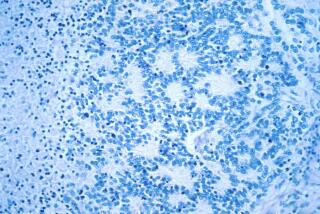
The gene in question is known as CCR5, and scientists suspect it plays a key role in ushering HIV into cells. Those who have two copies of a version of the gene known as CCR5 Delta32 appear to be resistant to HIV infection.
It took considerable effort, but the researchers were able to find a donor who fit the bill. Following customary treatment protocols for blood cancers, doctors killed off and suppressed much of the patientâs original immune system, then transferred a collection of stem cells drawn from the donorâs bone marrow.
Sixteen months after receiving the transplant, the patientâs immune system had fully incorporated the new pair of CCR5 genes. He was stable enough to see what would happen if he stopped taking his anti-retroviral drugs.
The answer: nothing. Even after 18 months, the London patient appeared to have suppressed the HIV virus completely, according to the Nature report.
While only time will tell whether his remission is permanent, the London patient looks to be cured of both his Hodgkinâs lymphoma and his HIV infection.
The study authors made clear that they donât expect stem cell transplants to become a standard treatment for HIV. As currently performed, largely in the treatment of blood cancers, the transplants are costly, complex and extremely dangerous.
Instead, the Berlin patient and the London patient offer important lessons about the genetic machinery that may act as a control switch for HIV. If adapted to immunotherapy and other treatments already coming into broad use, it could pave the way toward a cure.
The successful clearance of HIV in both men offers support for researchersâ long-held suspicion that having two copies of CCR5 Delta32 essentially knocks the gene out and prevents the most common form of HIV from entering a personâs cells to replicate itself.
âItâs quite clear that the CCR5 receptor is absolutely a critical part of what HIV needs to enter cells,â said Dr. Otto Yang, an infectious disease specialist and HIV researcher at UCLA. Turning that knowledge into an HIV cure will take many, many more steps, he added.
For starters, the HIV-1 virus adapts quickly to new environments and has proven adept at developing workarounds to survive. In efforts to replicate the success of the Berlin patient, a person with a greatly weakened remnant of HIV infection was treated and it was found that even then, the virus could roar back by using a second genetic program to enter cells and replicate. That person, dubbed the âEssen patient,â died.
Then there is the lingering uncertainty about the role a patientâs own immune system could play in vanquishing HIV.
Patients with deadly blood cancers generally undergo the near-total destruction of their own immune system to make way for donor stem cells. But even with a good match, a recipientâs own organs can come under attack by the newly transplanted cells, a phenomenon called graft-versus-host disease.
Researchers may try to skirt that outcome using techniques pioneered in the development of CAR-T cancer immunotherapies: They might harvest immune cells from an HIV patient, knock out the CCR5 gene that HIV needs to thrive, build up an army of altered cells and re-introduce them to the patient.
Such an approach could reduce the risk of graft-versus-host disease, Yang said. More importantly, it raises the question of whether itâs ideal â or even necessary â to wholly disable a patientâs immune system. Maybe with assistance from an immune-boosting agent, the reengineered cells could work with a patientâs original immune system to vanquish HIV infection, he said.
Gene therapy might be another way to go, said Dr. Jeffrey C. Laurence, an oncologist and HIV researcher at Weill Cornell Medicineâs Center for Blood Disorders in New York. This still-experimental approach would involve taking the machinery needed to produce cells with the desirable double mutation and ferrying it into a patient with the help of a virus.
Making HIV cures accessible to all will require even more hurdles to be cleared, Laurence added.
Even so, advances in gene editing, genetic engineering and immune therapies have made a cure seem possible, Sacha said.
âWe know we can do this,â he said.