Doctors: Cancer patients cured a decade after gene therapy

In 2010, doctors treated Doug Olsonâs leukemia with an experimental gene therapy that transformed some of his blood cells into cancer killers. More than a decade later, thereâs no sign of cancer in his body.
The treatment cured Olson and a second patient, according to the University of Pennsylvania doctors, who said it was the first time the therapy had been studied for so long.
âIâm doing great right now. Iâm still very active. I was running half-marathons until 2018,â said Olson, 75, who lives in Pleasanton, Calif. âThis is a cure. And they donât use the word lightly.â
His doctors describe the two cases in a study published Wednesday in the journal Nature. They say the two examples show the treatment, called CAR-T cell therapy, can attack cancer immediately, then stay inside the body for years and evolve there to keep the disease at bay. Such âliving drugsâ are now used by thousands around the world to treat certain blood cancers.
Based on the 10-year results, âwe can now conclude that CAR-T cells can actually cure patients of leukemia,â said Dr. Carl June, one of the study authors.
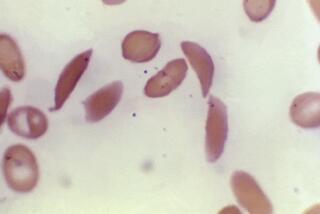
The one-time treatment involves collecting the patientâs T cells, white blood cells key to the immune system, and genetically changing them in the lab so that they will find and attack cancer cells. The modified cells are given back to the patient through IV.
By the time Olson got the treatment, heâd been fighting cancer for years. When doctors diagnosed him with chronic lymphocytic leukemia in 1996, he said, âI thought I had months to live.â
He eventually underwent chemotherapy and, at one point, his physician, Dr. David Porter, suggested he may need a bone marrow transplant. Porter also raised the idea of joining a CAR-T therapy study. Olson, chief executive of a New Hampshire lab products company, said he was excited by the science and eager to avoid the transplant.
A couple of weeks after getting the treatment, he felt sick for about a week and was hospitalized for three days.
âIt was the very next week he sat me down and he said, âWe cannot find a single cancer cell in your body,ââ Olson recalled.
The other patient, retired corrections officer Bill Ludwig, had similar results.
Over time, researchers said, the modified cells evolved, many turning into âhelperâ cells that work with the cancer-killing cells. Helper cells eventually became dominant in both patients.
Study author J. Joseph Melenhorst said they were able to isolate and analyze the cells using new technologies, which gave them âvery good insightâ into how they persisted in the patientsâ bodies.
Dr. Armin Ghobadi of Washington University in St. Louis, an expert in gene and cellular immunotherapy for cancer, called the findings âincredible.â Though the word âcureâ is rarely used in cancer, he said it appears these patients were âmost likelyâ cured.
In the all-hands effort to harness the powers of the immune system to fight cancer, scientists have reported a new approach that eliminated all evidence of advanced-stage breast cancer in a 49-year-old woman who had run out of treatment options.
He was intrigued by the persistence of the CAR-T cells and the way the living drug evolves.
âThatâs just really beautiful to see,â said Ghobadi, who was not involved in the study.
At this point, June said, tens of thousands of patients are being treated with CAR-T cell therapies, which have been approved for certain blood cancers by health authorities around the world, including the U.S. Food and Drug Administration. The agency first approved a CAR-T therapy treatment in 2017 developed by Penn and the drugmaker Novartis for childhood leukemia.
The Nature study was paid for partly by the Novartis Institute for Biomedical Research and partly by National Institutes of Health grants.
Scientists hope to see wider use of CAR-T therapies in the future for other cancers. Last year, a CAR-T cell therapy was approved for multiple myeloma, the most common malignancy of the bone marrow in adults. According to the Leukemia & Lymphoma Society, leukemia, lymphoma and myeloma were expected to make up just under 10% of the 1.9 million new cancer cases in the U.S. last year.
âBut the big scientific challenge â and itâs a big one â is how to make this work in solid cancers,â like those in the lung, colon and other places, June said.
Even in blood cancers, there are challenges. The therapies are expensive, running into the hundreds of thousands of dollars just for the drugs. And thereâs the risk of significant side effects, including an immune overreaction called âcytokine release syndromeâ and nervous system-related problems such as brain swelling.
Both of the Penn patients did extremely well after the treatment. Ludwig traveled the country with his wife in a motor home and celebrated family milestones before dying early last year of COVID-19 complications.
Olson said heâs extremely grateful for the decade of life since doctors used cutting-edge science to save him.
âWhatâs changed is the dimension of hope. The pace of discovery takes your breath away,â he said. âItâs a brand-new world.â
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.