Has California avoided another devastating winter COVID wave?

In the first two years of the COVID-19 pandemic, winter holidays were marred by a pair of devastating waves that ripped through California, sending case counts soaring, residents to the hospital in droves and, ultimately, leaving thousands dead.
But the third winter seems to have escaped that same fate. A late autumn upswing in transmission, which picked up steam after Thanksgiving, began to dissipate in mid- to late December instead of becoming the runaway train public health officials had feared. And in a stark departure from previous years, COVID-19 metrics have continued to improve in the weeks since.
Officials emphasize that the danger is not past â especially for those at higher risk of developing severe illness.
Thereâs also a chance another problematic variant could emerge. Officials are keeping a close eye on XBB.1.5, which has been described as the most infectious edition of the virus yet.
The latest Omicron subvariant, perhaps the most infectious yet, has gained a foothold in California. Officials say its growth advantage is worrisome.
But the fact that California navigated what was, for many, the closest thing to a normal holiday season since 2019, without a record-setting spike in infections or surge in hospitalizations, is cause for optimism â and it underscores the power of the tools at our disposal, experts say.
âI never say weâre in the clear, because thereâs still people for whom COVID is going to remain a really big concern, and theyâre going to continue to need to do everything they can to avoid getting infected,â Los Angeles County Public Health Director Barbara Ferrer said. âWe still have a lot of virus in our communities, but we are definitely in a promising place.â
How did this happen?
Many residents probably enjoyed some degree of protection against the coronavirus because they have been vaccinated, previously infected or both. This means some were able to avoid getting infected, while othersâ immune systems were better primed to ward off severe illness.
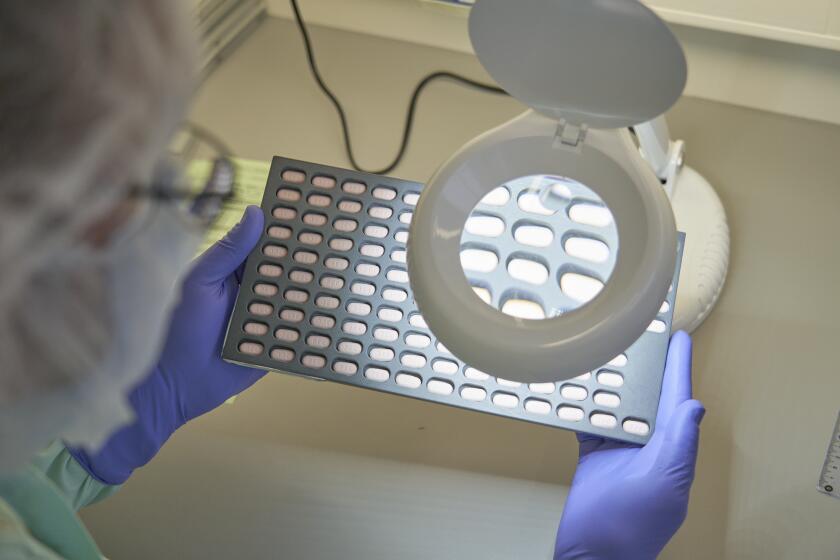
Anti-COVID drugs â including Paxlovid and another oral medication known as molnupiravir â also probably helped by keeping higher-risk individuals from falling seriously ill.
Drugs such as Paxlovid and molnupiravir are free and widely available, but officials say doctors are not prescribing them as much as they should.
Bivalent boosters, formulated specifically to help protect against the Omicron subvariants that have dominated in the last year, also became available in September. Uptake has been too slow for some officialsâ liking, but almost 24% of eligible Californians have received the updated dose.
âVaccinations, including bivalent boosters, can help protect you from getting seriously ill or even dying,â said Dr. Wilma Wooten, San Diego Countyâs public health officer.
Behavioral changes â including moving gatherings outside, testing before events, wearing a mask in indoor public settings and doubling down on hand-washing and other health hygiene efforts â also may have played a role.
âWhile nothing can be said with certainty, currently weâre seeing evidence that our tools to fight COVID-19, including masks, the bivalent booster and therapeutics, are working,â Ferrer said Thursday.
What do the numbers show?
Case counts across California have dropped steadily since the first week of December, and so have coronavirus levels in wastewater.
In L.A. County, wastewater levels began declining in early December, although in recent weeks, they have plateaued at about 70% of last summerâs peak â still a high level of concern, as defined by health officials.
âWhile wastewater concentration levels are not low, simultaneously, weâre not seeing the postholiday spike that was expected by the end of the first week in January,â Ferrer said.
The latest maps and charts on the spread of COVID-19 in California.
In San Diego County, Wooten said in a statement that âthe virus is still circulating in the region. Weâre still seeing high percentages of positive COVID-19 tests and detecting high levels of the virus in wastewater.â
Elsewhere, recent analysis âshows wastewater signals decreasing in the Greater Sacramento, San Joaquin Valley and Southern California regions, and plateauing in the Bay Areaâ and Northern California, the state Department of Public Health wrote in an update Thursday.
Other metrics also lend credence to the concept that coronavirus activity has slowed. Modeling from the California Department of Public Health estimates that the spread of COVID-19 is probably decreasing statewide and has been trending downward or stable for the last month.
Los Angeles County has seen marked improvement in its pandemic metrics. A much-discussed double COVID wave fueled by gatherings and travel has not materialized.
What about hospitals?
Though many infected with the coronavirus experience mild symptoms, or none at all, any pronounced uptick in transmission threatens to send a new wave of patients to hospitals. In 2020â21 and 2021â22, these deluges were massive and put immense pressure on healthcare systems across the state.
Although California did see a pronounced uptick in coronavirus-positive hospitalizations starting in late October and continuing through mid-December, that census has since plummeted.
On Thursday, 3,168 such patients were hospitalized statewide â a 29% drop in the last two weeks.
That figure includes those hospitalized with COVID-19-related illnesses and those who test positive incidentally after seeking care for some other reason.
Should there not be a significant resurgence of COVID-19 this winter, it will be the first time since the pandemic began in 2020 that a fall-and-winter wave was less severe than the preceding summerâs, in terms of hospitalizations.
Using machine learning, scientists have trained computers to comb the internet and recognize the early signs of a COVID-19 surge up to 6 weeks in advance.
Continued improvements have prompted a parade of California counties to progress to the low COVID-19 community level, as defined by the U.S. Centers for Disease Control and Prevention.
Placement in that category hinges on recent calculations of coronavirus case and hospitalization rates, as well as bed occupancy, and indicates that the burden on hospitals is relatively mild.
Fourteen California counties moved into the low COVID-19 community level Thursday: Alameda, Butte, Contra Costa, Fresno, Glenn, Humboldt, Kern, Kings, Los Angeles, Madera, Marin, Sonoma, Tehama and Ventura.
With last weekâs update, 71% of Californians now live in counties with a low COVID-19 community level, up from 28% the prior week.
Long COVID is characterized by a range of health problems that can last for months. In some cases, symptoms have lingered for a year or more.
Deaths remain a concern
As of Jan. 10, California was reporting 355 COVID-19 deaths per week. Although that has increased lately, it remains below the summer peak of 396 and far below last winterâs peak, when 1,827 deaths were recorded for the week ending Feb. 27.
More than 98,000 Californians have died from COVID-19, a toll that exceeds the entire population of cities such as Santa Monica, Mission Viejo and Redding.
Nationally, COVID-19 is responsible for far more deaths than flu. The CDC has reported more than 44,000 COVID-19 deaths since the start of October, more than double the estimated 17,000 from flu.
The move to treat COVID-19 more like influenza would further relax mask wearing and other preventive measures as the country seeks to return to normality.
What about XBB.1.5?
XBB.1.5 is among the latest alphanumerical members of the sprawling Omicron family. Itâs a descendant of XBB, which is a recombinant of descendants of the Omicron subvariant BA.2.
Much of the focus surrounding this particular subvariant has been its infectivity, as it may be the most transmissible version of the coronavirus.
XBB.1.5 now accounts for an estimated 49.1% of all new cases in the U.S., making it the most common edition of the coronavirus in circulation nationwide, according to the CDC.
Though its share has grown steadily, it remains far less common in the region that includes California, Nevada, Arizona, Hawaii and the Pacific island territories. An estimated 24.1% of coronavirus cases over the last week were thought to be XBB.1.5, CDC data show.
The distressing development comes even as other metrics show a relatively promising picture, including a decrease in case counts.
The ultimate effect of XBB.1.5 in terms of hospitalizations remains unclear. But current data suggest the new variant is not fueling a spike.
For instance, Ferrer said, Atlanta is in a region where about 31% of coronavirus specimens were estimated to be XBB.1.5. Thatâs double what it is for the region that includes Chicago.
If XBB.1.5 were fueling a surge in hospitalizations, youâd expect the Atlanta areaâs hospitalization rate to be worse than the Chicago areaâs. Yet the latterâs hospitalization rate â 11.1 new weekly coronavirus-positive hospitalizations for every 100,000 residents in Cook County â has been higher than Atlantaâs Fulton County, which has a hospitalization rate of 8.8, Ferrer said.
She noted, however, that âthere are a lot of underlying variables that are affecting hospitalization rates in different regions â including local policies, vaccination rates and even behaviors that change according to the weather, such as being inside more.â
âWhile we need to continue to track the impact of increased circulation of XBB and XBB.1.5 on illness severity, the current information suggests that this strain of Omicron is not having a major impact on hospitalization rates as of this time,â Ferrer said.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.