First COVID-19 vaccines should go to healthcare workers and nursing homes, panel says

Healthcare workers and nursing home residents should be at the front of the line when the first coronavirus vaccine shots become available, an influential government advisory panel said Tuesday.
The panel voted 13-1 to recommend that those groups get priority in the first days of any coming vaccination program, when doses are expected to be very limited. The two groups account for about 24 million people out of a U.S. population of about 330 million.
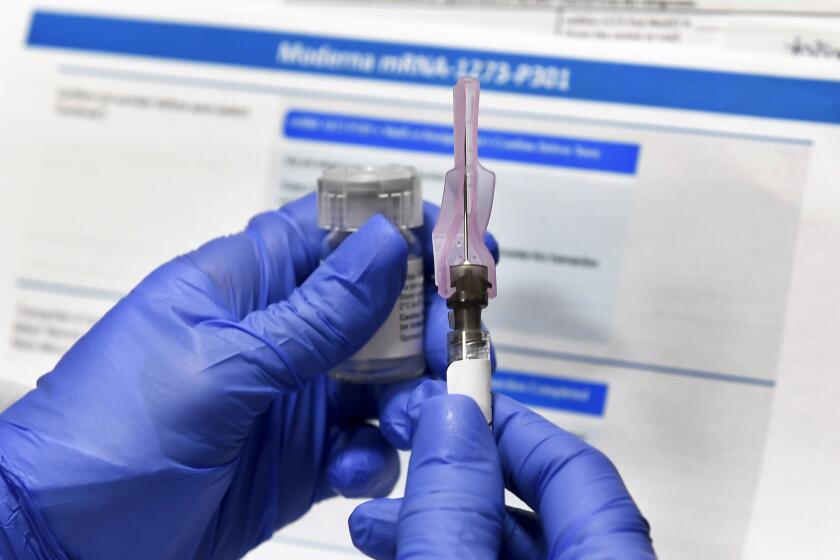
Later this month, the Food and Drug Administration will consider authorizing emergency use of two vaccines made by Pfizer and Moderna. Current estimates project that no more than 20 million doses of each vaccine will be available by the end of 2020. And each product requires two doses. As a result, the shots will be rationed in the early stages.
Gov. Gavin Newsom has announced a stay-at-home order affecting most of California.
The Advisory Committee on Immunization Practices will meet again to decide who should be next in line. Among the possibilities: teachers, police, firefighters and workers in other essential fields such as food production and transportation; the elderly; and people with underlying medical conditions.
Tuesdayâs action merely designated who should get shots first if a safe and effective vaccine becomes available. The panel did not endorse any particular vaccine. Panel members are waiting to hear the FDAâs analysis and to see more safety and efficacy data before endorsing any particular product.
Experts say the vaccine will probably not become widely available in the U.S. until the spring.
When people talk about COVID-19 vaccines, they can sound like theyâre speaking a foreign language. Donât worry! Hereâs your guide to vaccine vocabulary.
The panel of independent scientific experts, created in 1964, makes recommendations to the director of the Centers for Disease Control and Prevention, who almost always approves them. It normally has 15 voting members, but one seat is vacant.
The recommendations are not binding, but for decades they have been widely heeded by doctors, and they have determined the scope and funding of U.S. vaccination programs.
It will be up to state authorities whether to follow the guidance. It will also be left to them to make further, more detailed decisions if necessary â for example, whether to put emergency room doctors and nurses ahead of other healthcare workers if vaccine supplies are low.
The outbreak in the U.S. has killed nearly 270,000 people and caused more than 13.5 million confirmed infections, with deaths, hospitalizations and cases rocketing in recent weeks.
As the virtual meeting got underway, panel member Dr. Beth Bell of the University of Washington noted that on average, one person is dying of COVID-19 per minute in the U.S. right now, âso I guess we are acting none too soon.â
Federal regulators will consider requests in December by Pfizer and Moderna for emergency use authorization for their coronavirus vaccines.
About 3 million people are living in nursing homes, chronic care hospitals, and other U.S. long-term care facilities. Those patients and the staff members who care for them have accounted for 6% of the nationâs coronavirus cases and 39% of the COVID-19 deaths, CDC officials say.
Despite the heavy toll, some board members at Tuesdayâs meeting said they hesitated to include such patients in the first group getting shots.
Dr. Helen Keipp Talbot, an infectious diseases researcher at Vanderbilt University who was the lone committee member to vote against the proposal, cited influenza research that found vaccinating the staff of such facilities has the greatest impact on preventing its spread there.
Dr. Richard Zimmerman, a University of Pittsburgh flu vaccine researcher who watched the meeting online, echoed Talbotâs concerns.
âI think it was prematureâ to include nursing home residents as a priority group, said Zimmerman, a former ACIP member. âTheir vote seems to assume that these people will respond well to the vaccine. ... I donât think we know that.â
California and other states are racing to finalize plans for who will get the first doses of COVID-19 vaccines and how they will be delivered.
Committee members were unanimous in voicing support for vaccinating healthcare workers â about 21 million people, according to CDC officials.
That broad category includes medical staff who care for â or come in contact with â patients in hospitals, nursing homes, clinics and doctorâs offices. It also includes home healthcare workers and paramedics.
Depending on how state officials apply the panelâs recommendations, it could also encompass janitorial staff, food service employees and medical records clerks.
The government estimates people working in healthcare account for 12% of U.S. COVID-19 cases but only about 0.5% of deaths. Experts say itâs imperative to keep healthcare workers on their feet so they can administer the shots and tend to the ballooning number of infected Americans.
For months, members of the immunization panel had said they wouldnât take a vote until the FDA approved a vaccine, as is customary. But late last week, the group scheduled an emergency meeting.
The panelâs chairman, Dr. Jose Romero, said the decision stemmed from a realization that the states are facing a Friday deadline to place initial orders for the Pfizer vaccine and determine where they should be delivered. The committee decided to meet now to give state and local officials guidance, he said.
But some panel members and other experts had also grown concerned by comments from Trump administration officials that suggested differing vaccine priorities.
Distributing COVID-19 vaccine will be biggest health operation in L.A. history. Can the bureaucracy pull it off?
Dr. Deborah Birx of the White House coronavirus task force said in a meeting with CDC officials last month that people 65 and older should go to the head of the line, according to a federal official who was not authorized to discuss the matter and spoke to The Associated Press on condition of anonymity.
Then last week, U.S. Health and Human Services Secretary Alex Azar stressed that ultimately governors will decide who in their states gets the shots. Vice President Mike Pence echoed that view.
Asked whether Azarâs comment played a role in the scheduling of the meeting, Romero said; âWe donât live in a bubble. We know what he said. But that wasnât the primary reason this is being done.â
Jason Schwartz, a professor of health policy at the Yale School of Public Health, said it makes sense for the panel to take the unusual step of getting its recommendation out first.
âWithout that formal recommendation, it does create a void from which states could go off in all sorts of different directions,â said Schwartz, who is not on the panel.
There are still many unknowns when it comes to the pandemic, but the early signs of success for two experimental COVID-19 vaccines make a few things clear.
HHS officials have said they will distribute initial doses to states based on population, and itâs possible that some states wonât receive enough to cover all of their healthcare workers and nursing home residents.
CDC officials said they are optimistic such shortages would last only a few weeks.
Still, governors and local officials may have to decide which healthcare workers or regions get shots first, Schwartz said.
âItâs up to states to figure out the more granular detail,â he said.