Should Medicare pay for brain scans to detect Alzheimerās? Study results are mixed
A big study to help Medicare officials decide whether to start covering brain scans to check for Alzheimerās disease missed its goals for curbing healthcare costs, calling into question whether the pricey tests are worth it.
The results, announced this week, come from a $100-million study of more than 25,000 Medicare recipients. The study has been closely watched by private insurers too, as the elderly population grows and more Americans develop this most common form of dementia, which currently has no cure.
Advocates for coverage say they hope to persuade the agency that the scans still offer benefits even if they donāt save much ā or any ā money. For example, an accurate diagnosis helps families plan for the future even if the course of the disease canāt be changed, said study leader Dr. Gil Rabinovici of UC San Franciscoās Memory and Aging Center.
The study results were presented at the Alzheimerās Assn. International Conference taking place online because of the COVID-19 pandemic. They have not yet been reviewed by other scientists or published in a medical journal.
A spokesman for the Centers for Medicare and Medicaid Services said the agency considers all information on risks and benefits, and that a formal request would need to be filed to prompt reconsideration of its 2013 decision to not cover the scans except in research and special circumstances.
An experimental blood test was highly accurate at distinguishing people with Alzheimerās from those without it in several studies, scientists report.
More than 5 million people in the United States and millions more worldwide have Alzheimerās disease. The only certain way to diagnose it used to be checking a patientās brain after death.
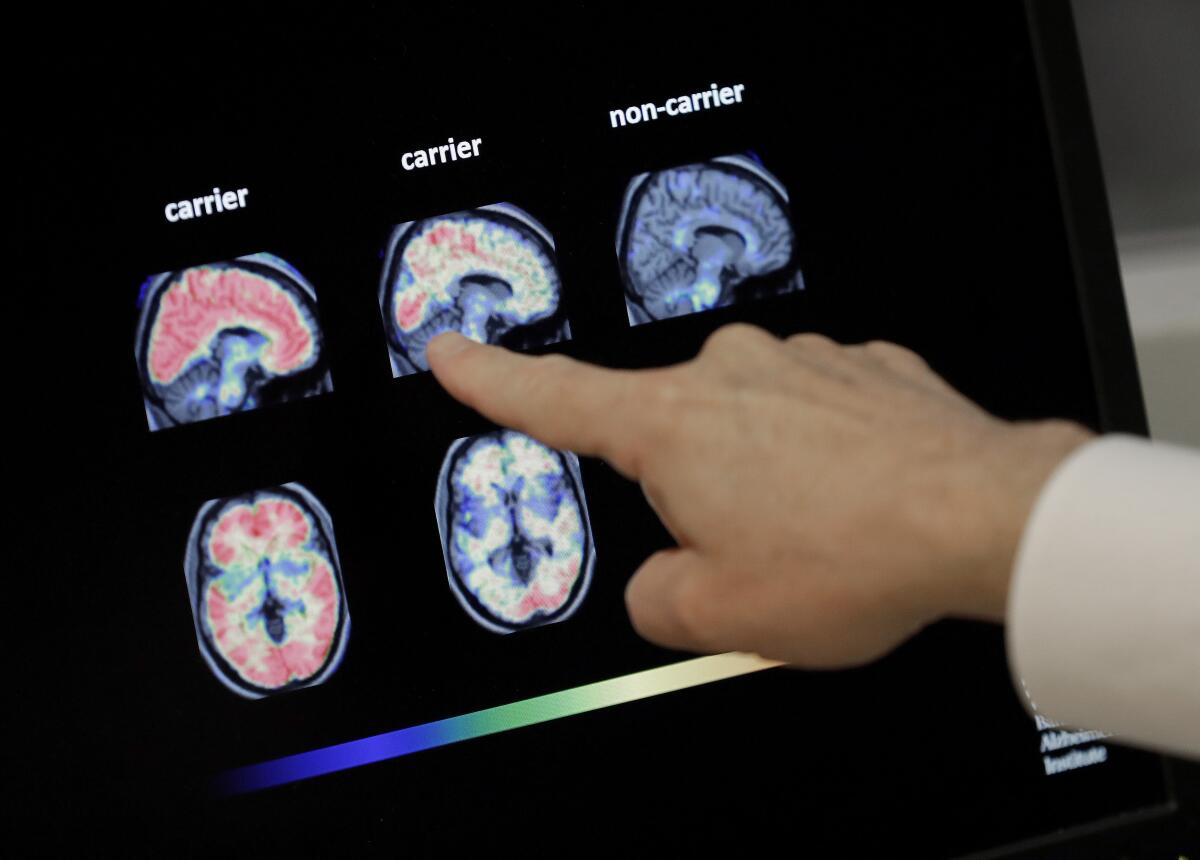
Recently, PET brain scans have been developed to detect signs of the disease in living patients. But they cost $4,000 to $5,000, and insurers havenāt covered them because itās not known if they have benefits.
The Imaging Dementia ā Evidence for Amyloid Scanning, or IDEAS, study aimed to find out. It involved 12,684 people with dementia or a less severe condition called mild cognitive impairment, or MCI. They were given scans and compared to Medicare recipients who were similar in age, sex and other factors but not given scans.
Partial results from the first 4,000 participants a few years ago suggested the scans more accurately diagnosed Alzheimerās disease and altered counseling or care in up to 60% of cases.
This part of the study examined whether the scans save money by reducing hospitalizations and emergency room visits. These are high among people with dementia because their confusion may lead them to take too much medicine or skip them altogether, or to fall and break a bone. In theory, a scan that could determine that someone has Alzheimerās would allow caregivers to take steps to prevent such problems.
The study missed its goal of curbing hospitalizations by 10% in the year after the scan: Rates were 24% among those scanned versus 25% of the others.
However, among those scanned, there were fewer hospitalizations for those with Alzheimerās versus those without the disease.
That result suggests that caregivers āwerenāt panickingā when they saw symptoms that could be due to Alzheimerās and didnāt rush to the hospital, said Maria Carrillo, the Alzheimerās Assn.ās chief science officer.
The association sponsored the study with the American College of Radiology and several imaging companies. Medicare officials helped design it and paid for the scans. Rabinovici is a paid advisor to several companies developing Alzheimerās treatments or diagnostics.
The first wave of coronavirus vaccines might be like a flu shot, experts say, curbing symptoms in some patients but not protecting them from COVID-19.
Dr. Suzanne Schindler, a neurologist at Washington University in St. Louis who enrolled patients in the study, said that with no treatment to alter the course of the disease, āitās a very fair question ā why should we even do this testing?ā
But patients and families want an accurate diagnosis to make big life decisions such as whether to move, retire or shift their finances, she said.
That was the case for Keith Szolga, whose 83-year-old mother, Beverly Szolga, had a scan at Washington University. Doctors had ruled out some other possible causes for her growing confusion and the scan showed Alzheimerās.
After getting the results, āI donāt think that we did much of anything differently other than we no longer let her drive,ā Keith Szolga said. āIt gives family members peace of mind to knowā what theyāre up against.
Dr. Howard Fillit, chief science officer of the Alzheimerās Drug Discovery Foundation, which had no role in the study, sees value in the scans.
āIf it was any other disease, people would want a specific diagnosisā and the scans give that, he said.
But with a blood test on the horizon for diagnosing the disease, relying on scans āmay become a moot issue,ā he said.








