Threat from food-borne illnesses shifts to new pathogens, CDC report says
The risk of infection from Salmonella-tainted food Salmonella fell in 2014, but strains of the bacterium still had the highest incidence among all pathogens tracked public health officials, a new report says.
The risk of infection from eating food tainted with a common type of salmonella or a dangerous strain of E. coli fell significantly in 2014, according to a report published Thursday by the U.S. Centers for Disease Control and Prevention.
That’s the good news. The bad news is that rates of infection with other types of pathogens – including bacteria such as Campylobacter and Vibrio – are on the rise.
Overall, the incidence of food-borne infections in the U.S. was about the same in 2014 as it was for 2006-08, a baseline period that coincided with an E. coli outbreak tied to tainted spinach that sickened at least 205 people and caused three deaths.
“Progress has been made in decreasing contamination of some foods and reducing illness caused by some pathogens,” says the report in the CDC’s Morbidity and Mortality Weekly Report. “However, little or no recent reductions for most infections have occurred.”
For the full year, the Foodborne Diseases Active Surveillance Network identified 19,542 infections associated with contaminated food, including 4,445 hospitalizations and 71 deaths. These laboratory-confirmed infections occurred in the 10 states that are part of the network, known as FoodNet.
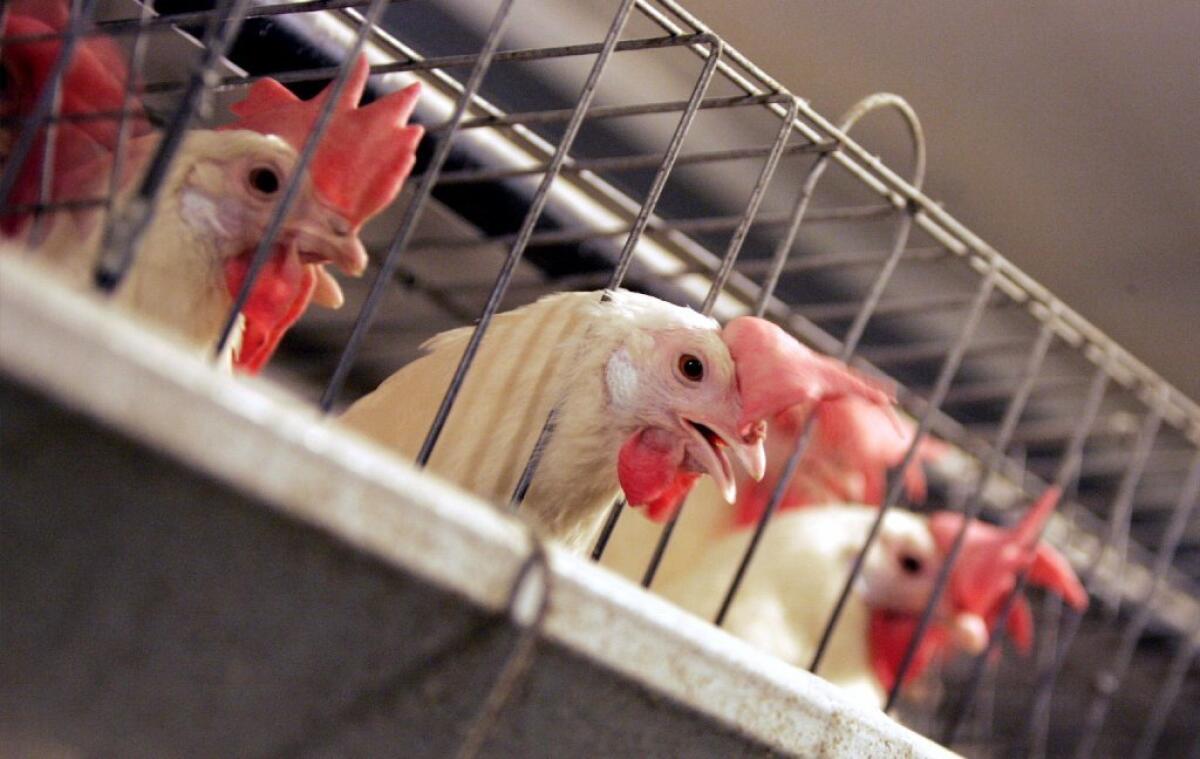
Salmonella was the top culprit in food-borne illnesses, with an incidence of 15.45 infections per 100,000 people, the report says. In 2014, various strains of the wily bacterium caused outbreaks in cucumbers, bean sprouts, chia powder and raw cashew cheese. It also caused outbreaks in Tyson chicken, backyard poultry flocks and pet bearded dragons.
Campylobacter was a close second, with an incidence of 13.45 infections per 100,000 people. This bacterium turned up in raw milk in Wisconsin and Utah, along with chicken livers and oysters, according to Seattle attorney Bill Marler, who specializes in cases involving food-borne illnesses.
Toward the other end of the spectrum, the incidence of infection with Escherichia coli 0157 was a mere 0.92 cases per 100,000 people in 2014. That was 32% lower than in the 2006-08 period, the biggest decline for any of the pathogens tracked in the report.
The study authors said this progress was the result of hard-fought efforts since the 2006 spinach outbreak to contain this particularly dangerous strain of E. coli. The bacterium makes a toxin that can cause bloody diarrhea and kidney failure, both of which can be deadly.
E. coli 0517 typically enters the food supply on leafy vegetables or in beef, and producers in both of these industries have made changes to their production processes to prevent contamination, according to the report. Updated government regulations have played a role too. Rapid DNA fingerprinting of bacteria samples from patients has helped epidemiologists get to the bottom of outbreaks more quickly, allowing contaminated food to be recalled faster than in the past.
The other big success was with the typhimurium strain of salmonella, which caused 1.67 illnesses per 100,000 people in 2014. That incidence was 27% lower than in 2006-08, according to the report. Poultry producers have increasingly embraced salmonella vaccines and taken other steps to reduce contamination, but some of the reasons for the decline remain unclear, the authors wrote.
But the spread of other pathogens has made up for these gains. The incidence of illness tied to Vibrio was 52% higher in 2014 than in 2006-08, and it was 13% higher for campylobacter. In addition, two strains of salmonella were up sharply over this time period – infantis (162%) and javiana (131%).
“Despite ongoing food safety efforts, the incidence of many infections remains high,” the report authors wrote. “Further prevention measures are needed to make food safer and achieve national health objectives.”
They noted that the FDA is set to publish new rules to improve the safety of produce, processed foods and imported foods this year, in accordance with the Food Safety Modernization Act.
The FoodNet surveillance system covers about 48 million Americans who live in Oregon, New Mexico, Minnesota, Tennessee, Georgia, Maryland, Connecticut and parts of California, New York and Colorado -- about 15% of the U.S. population.
Public health officials from these 10 states work with the CDC, the U.S. Department of Agriculture and the Food and Drug Administration to monitor nine pathogens known to cause food-borne illnesses.
Follow me on Twitter @LATkarenkaplan and “like” Los Angeles Times Science & Health on Facebook.







