Could this drug help the brain recover after a stroke?
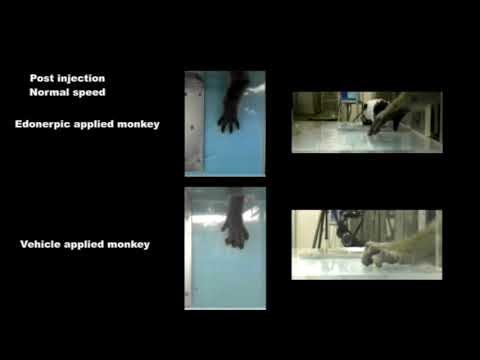
This video shows how an experimental drug called edonerpic maleate helped monkeys recover after a stroke, compared with a control group that did not get the drug. (Credit: H. Abe et al., Science, 2018)
Despite years of effort, researchers have so far failed to find a pill you could take or a food you could eat to harden your brain against the injury that could be caused by a stroke.
But new research offers the prospect of limiting a strokeâs long-term damage in a different way: with a drug that enhances the brainâs ability to rewire itself and promote recovery in the weeks and months after injury.
In experiments, both mice and macaque monkeys that suffered strokes regained more movement and dexterity when their rehabilitative regimen included an experimental medication called edonerpic maleate.
The drug, which has already run a gauntlet of safety trials as a possible medication for Alzheimerâs disease, appears to have enhanced the effectiveness of rehab by strengthening the connections between brain cells and nourishing the chemical soup in which those cells forge those new connections.
A report on the experiments appears in Fridayâs edition of the journal Science. The work was conducted by researchers at Yokohama City University School of Medicine and employees of Toyama Chemical Co., Ltd., a Japanese pharmaceutical firm that owns intellectual property rights to edonerpic maleate. Toyama provided funding for Yokohama City University to study the drug in macaque monkeys.
The findings from the mice shed important light on how edonerpic maleate may work in an injured brain.
But many experimental drugs have been effective in improving mobility in mice after a stroke, yet failed to work as well in primates. The fact that this one also improved movement in stroke-affected monkeys is evidence that it âmay be a strong candidateâ to help humans recover from a stroke, and possibly traumatic brain injury as well, the researchers said.
A stroke occurs when a blood vessel in the brain is blocked or ruptured, depriving a portion of the brain of oxygen and causing the death of affected brain cells. Even after oxygen is restored, permanent damage usually remains, often involving the loss of mobility and dexterity.
The most common kind of stroke is an ischemic stroke, in which blood flow is compressed or cut off by a clot or other blockage. In a hemorrhagic stroke â the kind the studyâs authors induced in monkeys â bleeding into the brain shuts off oxygen to cells and causes them to die.
For the 800,000 patients who have a stroke and the 1.7 million who suffer a traumatic brain injury each year in the United States, recovery can be arduous, miraculous and uncertain.
But neurologists and rehabilitation specialists have discerned a common pattern in most patientsâ trajectory of recovery. Patients typically take back much of the lost speech, movement and intellectual function they will regain in the first weeks and months after their injury, even though brain cells that have died are gone forever.
On their own and in response to rehabilitation, a patientâs surviving brain cells will work overtime to devise work-arounds. Theyâll lash themselves together to create new pathways for electrical signals, and a patient will often regain many lost skills. This ability of the brain to ârewireâ itself is called âplasticity,â and the better it works, the more function can be regained.
At a certain point, however, recovery will begin to plateau. Any motor, speech and intellectual skills that have been lost may stay lost.
Scientists have spent years looking for neuroprotective agents that can buffer the brain against the initial whack of a stroke, but theyâve had little success. Thatâs why a therapy that turbocharges this process of building back neuroplasticity after a stroke could be uniquely welcome.
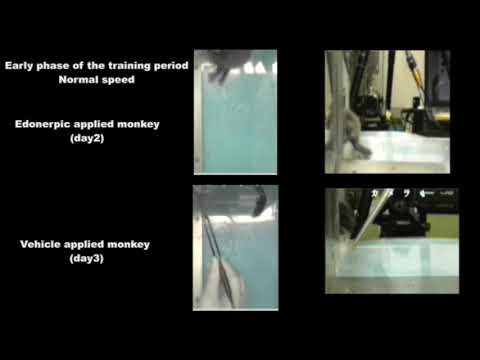
Another example of how an experimental drug callededonerpic maleate aided the recovery of macaques after a stroke. (Credit: H. Abe et al., Science, 2018)
The Japanese researchers tested edonerpic maleate by inducing hemorrhagic strokes in six macaques. One to two weeks later, the monkeys had recovered enough mobility to begin a series of exercises designed to mimic the rigors of stroke rehabilitation.
At this point, three of the monkeys were administered the drug 15 minutes before their therapeutic sessions. Compared to three monkeys that didnât get the drug, the ones that did experienced a greater degree of functional recovery.
For instance, they performed better in reward-retrieval exercises that required greater coordination of their arms and fine-motor function. And while the monkeys in the control group rarely recovered their ability to use a âprecision gripâ to grasp treats, the treated monkeys âfrequently showed dexterous hand movements,â the researchers reported.
UCLA neurologist Jason D. Hinman, who did not work on the new research, welcomed the results. He said edonerpic maleate is one of many therapies being tested to augment the effects of post-stroke rehabilitative therapy.
Other approaches include the use of robotics and other types of brain-machine interfaces to restore the flow of messages to a patientâs limbs; encouraging stem cells to grow new connections between surviving neurons; and a range of medications. In mice, the Alzheimerâs disease drug memantine (marketed as Namenda) has shown promise.
âWhatâs interesting about this approach is that, while thereâs some spontaneous recovery of function, itâs meant to be activated by rehabilitative therapy,â Hinman said. âIf you just sit on the couch, you donât get the benefit.â
With a drug that makes cells in an injured brain more active, Hinman cautioned, a runaway electrical event â in other words, a seizure â is one obvious safety concern.
Early research on endonerpic maleate had suggested it might protect neurons against the toxic build-up of the protein beta-amyloid, a hallmark of Alzheimerâs disease. Two rounds of clinical trials bolstered its safety record in humans.
Only after that, in July 2017, did Toyama Chemicalâs parent company, Fujifilm Corp., announce that the drug had failed to help patients with mild- to moderate Alzheimerâs.
Its side effects included diarrhea, nausea, dizziness and headache, and it may have caused two âserious adverse eventsâ in human trials, researchers reported at the time.
Many stroke patients either donât get the clot-busting drug tissue plasminogen activator (or tPA), which can lessen the impact of strokes, or they donât get to a hospital quickly enough for tPA to be tried.
Often debilitated by impairments, âthese patients are desperate for new treatments, so many would accept those risks,â Hinman said.
To read this article in Spanish, click here
MORE IN SCIENCE
Surprise! Scientists find signs of new brain cells in adults as old as 79
This retinal implant may one day cure blindness caused by macular degeneration
A sudden loss of wealth may be hazardous to your health







