Coronavirus Today: Getting sick on purpose
Good evening. Iâm Karen Kaplan, and itâs Tuesday, July 5. Hereâs the latest on whatâs happening with the coronavirus in California and beyond.
As a piece of advertising, it was certainly effective.
The ad pictured attractive young adults with backpacks and earbuds. In a sign of the times, they wore face masks and stood apart from one another. Instead of selling a product, they were making an appeal: âHelp us fight COVID-19.â
Nearly 37,000 people responded, including a 22-year-old from Birmingham, England, named Jacob Hopkins. He saw it as a way to help get the world back to normal faster.
Hopkins had been studying Cold War history at Newcastle University when Britain imposed its first pandemic lockdown and put his life on hold. He was eager for the pandemic to be over â he was living with his parents, working in a grocery store and unable to go backpacking abroad or hang out with his friends.
The possibility that he could play a small part in this historical moment gave him a sense of mission, he told my colleague Melissa Healy.
Thatâs how he wound up in a London hospital room with his head tilted back as doctors dribbled bits of SARS-CoV-2 into his nostrils. He was the first volunteer in a study designed to let researchers see how, where and for how long the coronavirus establishes itself in people.
âAll I did was sat in a room,â Hopkins said.

Actually, there was more to it than that.
The room was in St. Maryâs Hospital in London, and he was stuck there for 17 days. But he had frequent visitors â doctors, nurses and researchers in full personal protective equipment
who came in to draw blood and check his vital signs.
His duties as a human lab rat didnât end there. Each day included a battery of cognitive tests taken on a laptop, plus a âscratch-and-sniffâ smell test to gauge one of COVID-19âs signature symptoms. He also spent an hour wearing a plastic mask that measured his respiratory output.
Hopkinsâ plans to learn British sign language and catch up on movies gave way to more modest goals, such as playing video games and staring out the window at the London Eye. In fact, this existence became so mundane that the two occasions when he was bundled into a hazmat suit and wheeled to a CT scanner felt like ârare treatsâ because he got to see âsomething other than the four walls of a very sterile room,â he said.
He earned 4,565 British pounds (about $5,500) for his trouble, which included a commitment to return for follow-up visits.

The study included 35 more volunteers after Hopkins, none of whom became seriously ill. Thanks to them, researchers learned that even when people were given the lowest concentration of virus that could be measured in a lab, the median time it took for SARS-CoV-2 to establish itself in their throats was less than two days. On average, the viral load in patientsâ noses peaked five days after they were deliberately exposed, and they remained infectious for five more days â even if they never developed COVID-19 symptoms.
These and other findings were published this spring in the journal Nature Medicine, and more insights are expected to follow. They should aid in the development of future vaccines and COVID-19 drugs as well as guide health professionals who care for patients.
Studies like this â scientists call them âhuman challenge trialsâ â arenât widely accepted in the United States. Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, called them âPlan Dâ and an âabsolutely far-out contingency.â The risk that a healthy volunteer could become seriously ill or suffer long-term health effects just doesnât sit well here, although some doctors and bioethicists are advocating for the U.S. to see things the way the U.K. does.
Hopkins said his parents were âdefinitely not happyâ with his decision to catch the coronavirus for the sake of science. But he said heâd do it again in a heartbeat.
âI was so proud and happy to be a part of this,â he said. âI was really part of something special.â
By the numbers
California cases and deaths as of 3:43 p.m. Tuesday:
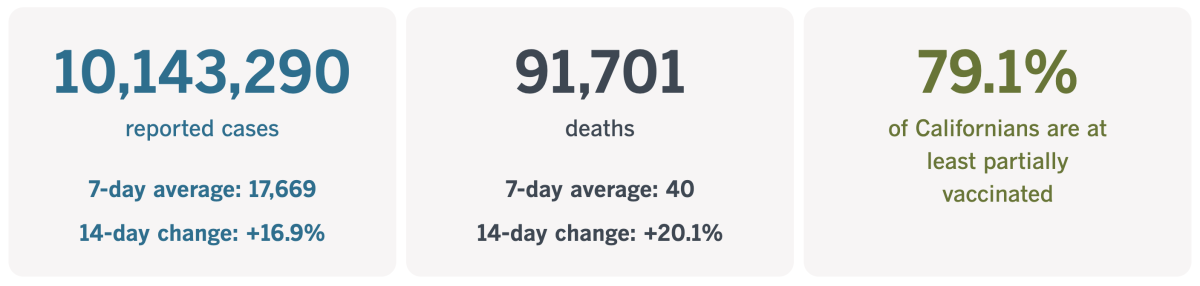
Track Californiaâs coronavirus spread and vaccination efforts â including the latest numbers and how they break down â with our graphics.
Quantifying COVID-19âs death toll
The higher the COVID-19 death toll climbs, the harder it is to comprehend. A new report from researchers at the National Institutes of Health makes it easier to digest the enormity of the loss.
The researchers examined U.S. death certificate data reported to the Centers for Disease Control and Prevention to determine the leading causes of death for most of 2020 and 2021. (In neither case do the data cover the entire calendar year â the analysis begins with March 2020, the first month of the pandemic era, and ends with October 2021, since data after that point were incomplete.)
COVID-19, a disease that didnât exist in the United States in 2019, was the third-leading cause of death in 2020 and again in 2021. Not only that, the No. 4 cause of death (accidents) wasnât even close:
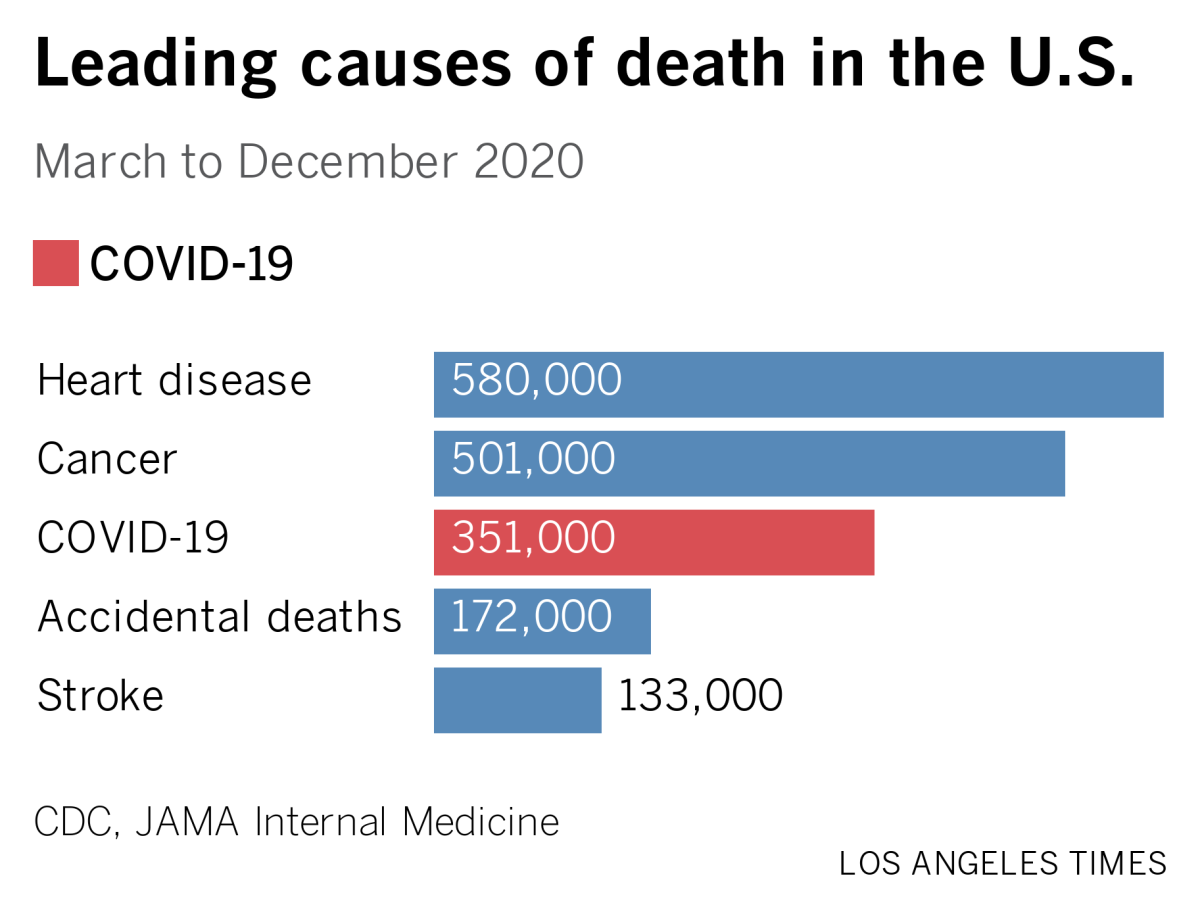
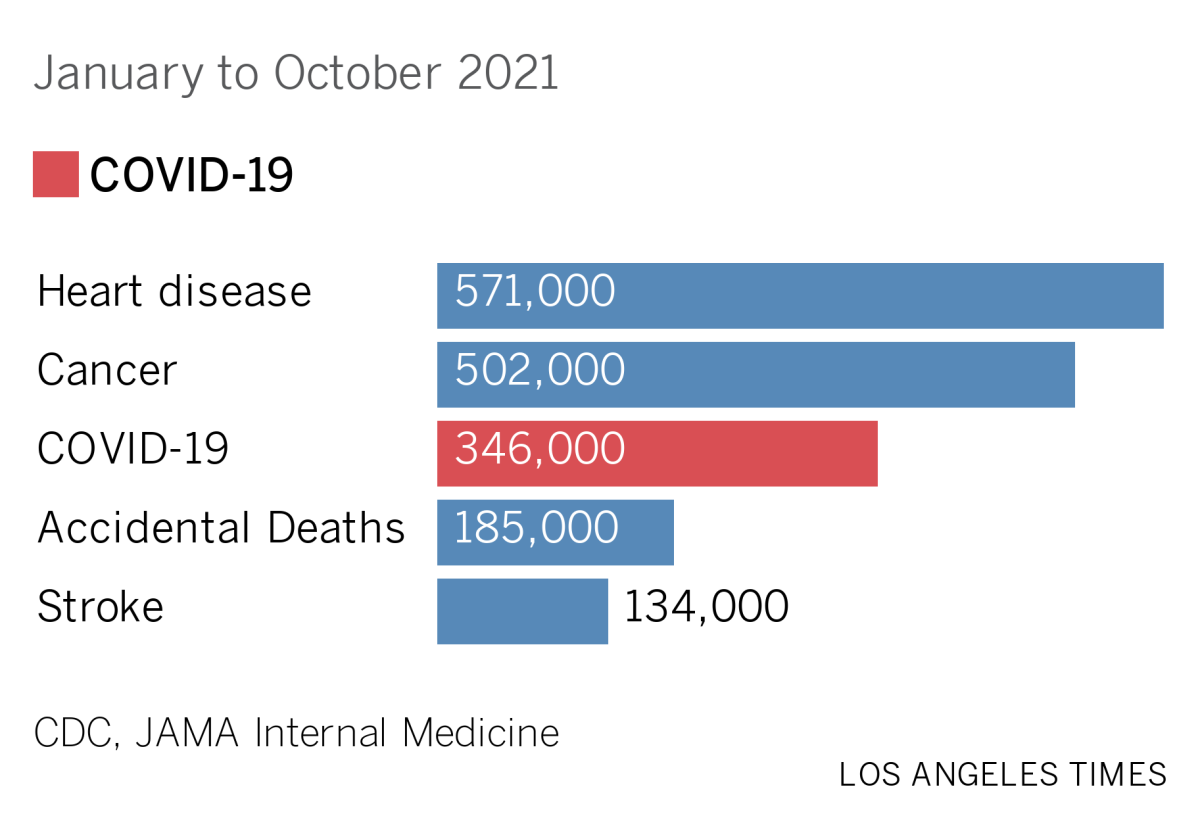
Hereâs an astounding statistic: Between March 2020 and October 2021, 1 out of every 8 deaths in the U.S. was due to COVID-19.
Hereâs another: If youâd turned 15 by the time the study period ended, your age group included COVID-19 among your top 5 causes of death. In fact, as of October 2021, COVID-19 was the No. 4 cause of death for 15- to 24-year-olds, as well as for 25- to 34-year-olds.
Then things got even worse: For Americans ages 35 to 44, COVID-19 was the No. 2 cause of death. And for those ages 45 to 54, COVID-19 was on top, killing 1,000 more people than heart disease and 2,000 more people than cancer.
With both of those age groups, the number of deaths due to other top killers â heart disease, cancer, accidents, suicide and chronic liver disease â was pretty stable between 2020 and 2021, rising or falling by no more than 3,000 year to year.
But COVID-19 was different. For those in the 35-to-44 age group, COVID-19 deaths increased from 6,100 in 2020 to 13,000 in 2021; for those 45 to 54, they increased from 17,000 to 30,000.
The sheer number of COVID-19 deaths increased for the next two age groups as well, from 42,000 to 60,000 for people ages 55 to 64, and from 76,000 to 85,000 for those ages 65 to 74.
COVID-19 deaths actually fell for Americans 75 and older. In 2020, there were 97,000 such deaths among 75- to 84-year-olds and 110,000 among those 85 and up. In 2021, the corresponding totals were 82,000 and 69,000. The authors suggested that the higher vaccination rates among the oldest Americans deserved credit for this reversal.
Bad as these numbers are, there are two reasons to presume the true picture is even worse. The first is that the 2021 tallies donât include any of the deaths from the devastating Omicron wave, which began after Thanksgiving. The second is that COVID-19 may have indirectly increased the number of fatalities due to heart disease, strokes, diabetes, accidents and Alzheimerâs disease by causing people to stay home when they should have sought medical treatment, the researchers wrote.
Their findings were published Tuesday by the journal JAMA Internal Medicine.

Another research group, from the University of Maryland and UC Irvine, examined COVID-19 deaths by county from the start of the pandemic through October 2021. They found that compared with counties that voted Democratic in the 2020 presidential election, counties that voted Republican had 73 more deaths per 100,000 residents.
Their calculation factored in the demographic and economic differences among counties, such as the fact that some had older (and presumably more vulnerable) populations, some had better access to healthcare resources, and some had higher COVID-19 vaccination rates.
Whatâs more, researchers observed a dose-response relationship. That means the bigger the margin for the Republican candidate, the higher the COVID-19 mortality rate per capita.
The early months of the pandemic didnât look this way. Initially, the response in both Democratic and Republican counties was largely the same, including lockdowns, school closures, mask mandates and capacity limits for indoor settings.
Some counties loosened these restrictions sooner than others, but it wasnât until early spring of 2021 â a few months into the COVID-19 vaccine rollout â that the link between voting records and cumulative mortality rates became large enough to qualify as statistically significant.
Of course, thereâs no inherent biological difference between Republicans and Democrats that would make one group more vulnerable to COVID-19.
âInstead, it appears that voting behavior acts as a proxy for compliance with and support for public health measures, vaccine uptake, and the likelihood of engaging in riskier behaviors (for example, unmasked social events and in-person dining) that could affect disease spread and mortality,â the researchers wrote in the June issue of Health Affairs.
âIt is likely that Democratic counties benefited more from public health guidance and mandates because residents were more willing to comply with those mandates, trust government messaging, and adhere to public health guidance,â they added.
Californiaâs vaccination progress
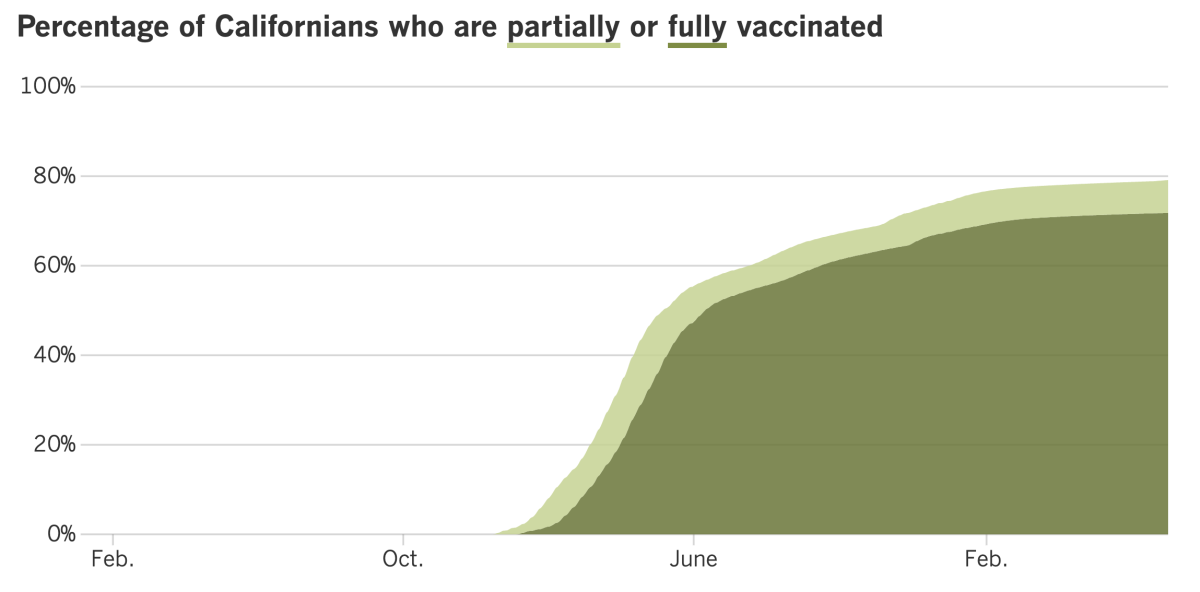
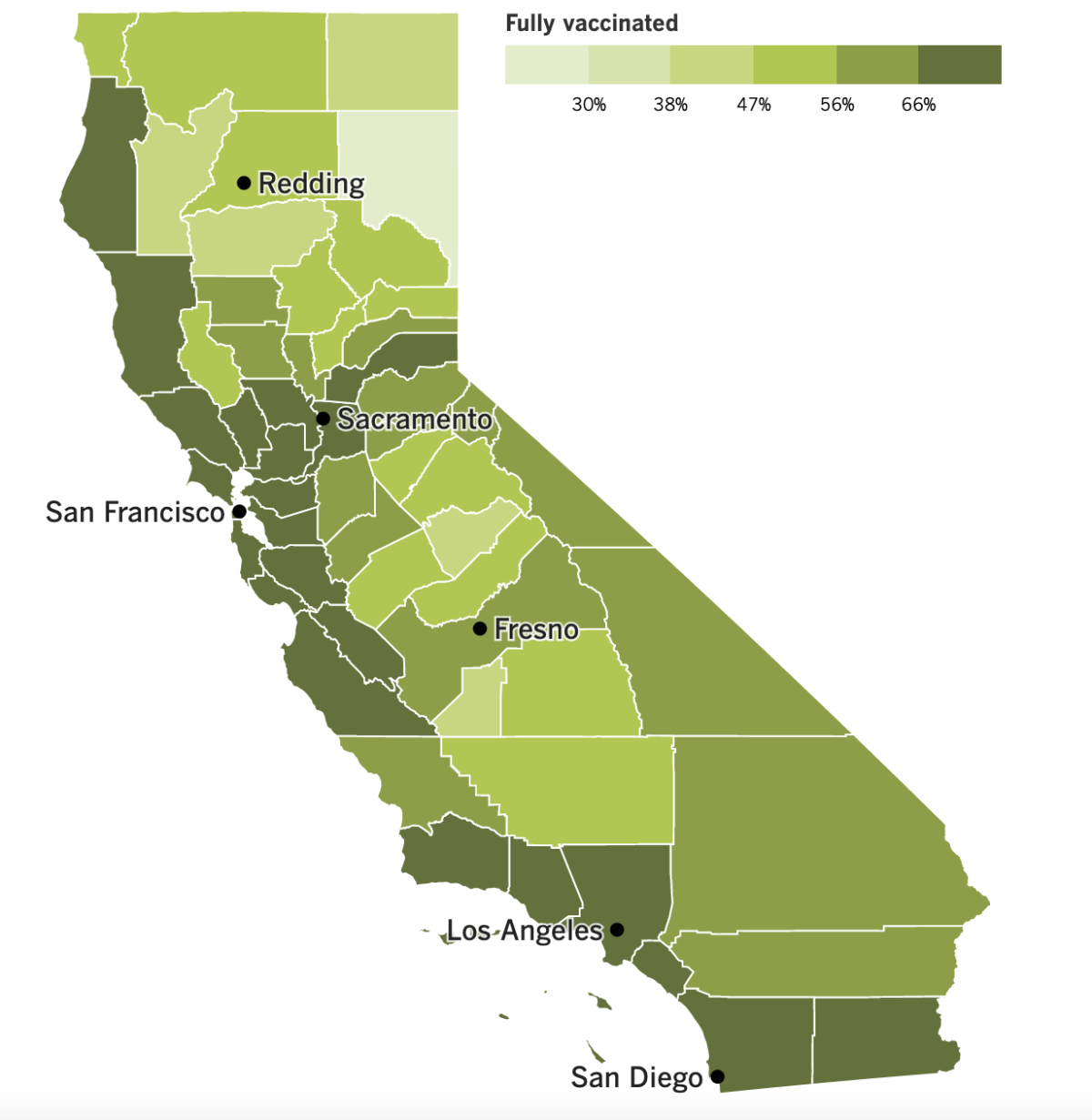
See the latest on Californiaâs vaccination progress with our tracker.
Your support helps us deliver the news that matters most.
In other news ...
You may have had a restful holiday weekend, but the coronavirus sure hasnât taken a break.
As of Thursday, 38 of Californiaâs 58 counties now meet the CDCâs criteria for having a high COVID-19 community level. They include the entire San Francisco Bay Area, the San Joaquin and Sacramento valleys, much of the rural northern part of the state, and Ventura County, the first in Southern California to achieve a high COVID-19 community level in the current Omicron wave.
Altogether, some 16 million Californians live in counties with a high COVID-19 community level. Thatâs 42% of the stateâs population. As recently as May, none of Californiaâs counties had a high COVID-19 community level.
Los Angeles County is still classified as âmedium,â but it has neighbors in the âhighâ category to its immediate north (Kern) and west (Ventura).
The CDC recommends that places in the âhighâ category implement a universal indoor mask mandate, something L.A. County Public Health Director Barbara Ferrer has said would happen here if the situation worsens from âmediumâ to âhigh.â
âWith the continued increase in cases, and now as youâre seeing the corresponding increase in hospitalizations ⌠weâre really worried,â she said.
The primary source of the current surge is no secret: Itâs the BA.5 subvariant of Omicron, which is getting a little help from its cousin BA.4.
Both strains are ultra-contagious. Ferrer said last week that âthereâs strong evidence they can spread even faster than other subvariants.â
But thatâs not their biggest superpower. Itâs that theyâre really good at infecting people who have already had the coronavirus, including cases caused by Omicron. That explains why folks like Xavier Becerra, who leads the U.S. Department of Health and Human Services, have gotten it twice in the span of a month.
âUntil recently, it was almost unheard of, but now itâs becoming more commonplaceâ to have COVID-19 two, three or even four times, said Dr. Eric Topol, head of Scripps Research Translational Institute. âIf we donât come up with better defenses, weâll see much more of this.â
Indeed, Topol called BA.5 âthe worst version of the virus that weâve seen.â
Nationwide, BA.5 accounted for nearly 54% of all SARS-CoV-2 viruses in circulation last week, according to the latest estimates from the CDC. Thatâs up from 40.5% the week before and 27% the week before that. As of last week, BA.4 was responsible for an additional 16.5% of COVID-causing coronaviruses on the loose.
BA.5 and BA.4 account for a similar share of the coronavirus soup in the region that includes California, Arizona, Nevada and Hawaii â 52% and 16.5%, respectively.
The rising number of cases isnât the only way to gauge the virusâ spread. In L.A. County, thereâs also been a substantial increase in the number of outbreaks tied to workplaces. To qualify as a workplace cluster, there have to be at least three documented infections within a two-week period.
Officials counted 301 âworksite case clustersâ in the week that ended Thursday, a 20% increase from the prior week. (For the sake of comparison, the previous week-to-week increase was 12%.) The last time the county saw so many workplace outbreaks at once was in early March.
In addition to the role of BA.5 and BA.4, Ferrer attributed the escalation to the fact that more employers are holding meetings and events indoors, a decline in mask use among employees, and the fact that some people are coming to work despite having symptoms of COVID-19.
Hereâs another sign of BA.5âs and BA.4âs outsize influence: The U.S. Food and Drug Administration has asked COVID-19 vaccine makers to produce booster shots for the fall that are specially formulated to target the two subvariants as well as the original coronavirus strain.
The FDA says people who are getting vaccinated for the first time should still get one of the original mRNA shots (either Comirnaty from Pfizer and BioNTech or SpikeVax from Moderna). But for some people at least, a fall booster might be a better match for the actual viruses theyâre likely to encounter.
Of course, that will only be the case if regulators have guessed correctly that BA.5 and BA.4 will remain the primary threats in the months to come. U.S. health officials make similar predictions when it comes to our annual flu shots, and some guesses are better than others.
Both Pfizer and Moderna had begun testing new boosters designed to counter the original version of Omicron. Now theyâll have to tweak their recipes again. If they perform well in tests, theyâll be evaluated by the CDC, which would then decide whether to recommend them to everyone or only to certain groups, such as older adults or people with compromised immune systems.
The Biden administration has announced a $3.2-billion deal to buy 105 million doses of Comirnaty for a fall booster campaign, with the option of buying up to 300 million doses. The order will include a mix of shots with doses for adults and children.
Since Congress remains gridlocked over Bidenâs multibillion-dollar request for more COVID-19 aid, the administration cobbled together the funds by reallocating money from earlier relief packages.
In South Korea, health officials have approved the countryâs first homegrown COVID-19 vaccine. SKYCovione from SK Bioscience performed better than the vaccine from AstraZeneca thatâs widely used abroad. Because it was designed with the original version of the coronavirus in mind, itâs not clear whether it will play a big role going forward.
And finally, the latest COVID-19 update from the World Health Organization says new coronavirus cases around the world increased 18% in the last week. Infections were increasing in 110 countries, mostly due to BA.5 and BA.4, said WHO Director-General Tedros Adhanom Ghebreyesus.
Deaths tied to COVID-19 were up in the Middle East, Southeast Asia and the Americas. In the previous reporting period, only one region â Southeast Asia â reported a small increase in deaths.
âThis pandemic is changing, but itâs not over,â Tedros said.
Your questions answered
Todayâs question comes from readers who want to know: If I get COVID-19, how long do I need to stay isolated?
First of all, the trigger for needing to isolate isnât having COVID-19, itâs testing positive for a coronavirus infection. If youâre infected but donât have any symptoms of disease, thereâs still a risk that you could spread the virus to someone else.
To plan your isolation, start by figuring out your âDay 0.â Thatâs the day of your first COVID-19 symptoms or the day you tested positive, whichever came first. The next full day counts as Day 1.
The CDC advises people who test positive to stay home for at least five full days, regardless of your vaccination status. If you donât live alone, you should stay away from other members of your household as much as possible. Whether youâre sick or merely infected, you should designate a âsick roomâ and stay there. If you can swing your own bathroom, be sure to do so.
If you must be around others, wear a high-quality mask that seals well to your face. Improving your ventilation â by opening windows and doors, deploying portable fans and exhaust fans, upgrading air filters and potentially using a portable air cleaner â will also help keep everyone safe.
If you experience certain troubling symptoms, you should seek medical attention right away. These include breathing problems, persistent chest pain or pressure, trouble waking or staying awake, confusion that wasnât evident before and changes in skin tone that have your skin, lips or nail beds looking pale, gray or blue.
The CDC says you can stop isolating after Day 5 if youâve gone 24 hours without a fever (without the help of medicines) and your other symptoms have improved. You donât have to be fully recovered, but you do have to keep wearing a high-quality mask for another five days. That means youâll need to avoid restaurants, gyms and other places where youâre likely to remove your mask.
If youâre still sick on Day 6, continue to isolate until youâve been fever-free for 24 hours without medication and your other symptoms are better. Keep wearing a mask through Day 10.
The advice from California health officials is almost exactly the same. The one exception is that isolation can end on Day 5 only if you take another coronavirus test and get a negative result. If you test positive, keep on isolating until Day 10 (or longer if youâre still sick).
Both California and the CDC recommend that you isolate, but L.A. Countyâs health order actually requires it. Other than that, the countyâs rules are in line with the stateâs advice.
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them. Wondering if your questionâs already been answered? Check out our archive here.
The pandemic in pictures

The little red Muppet in the photo above is Elmo, the 3½-year-old star of âSesame Street.â Now that kids in his age group are eligible to get vaccinated against COVID-19, he got his first dose last week and shared the news in a video.
âThere was a little pinch, but it was OK,â Elmo said in the public service announcement, which was posted on YouTube.
After Elmo went offscreen to look for a toy, his father, Louie (on the left), confessed to the camera that he had âa lot of questionsâ about the vaccine but felt reassured after talking to a pediatrician.
âI learned that Elmo getting vaccinated is the best way to keep himself, our friends, neighbors and everyone else healthy and enjoying the things they love,â said Louie, who was adorned with colorful bandages to match the green one on Elmoâs arm.
As of Tuesday afternoon, the video has been viewed more than 110,000 times.
Resources
Need a vaccine? Hereâs where to go: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get a test? Testing in California is free, and you can find a site online or call (833) 422-4255.
Americans are hurting in various ways. We have advice for helping kids cope, as well as resources for people experiencing domestic abuse.
Weâve answered hundreds of readersâ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




