Coronavirus Today: When outbreaks collide
Good evening. Iâm Russ Mitchell, and itâs Thursday, June 3. Hereâs whatâs happening with the coronavirus in California and beyond.
As if dealing with the COVID-19 pandemic werenât bad enough, now scientists are becoming concerned about the possibility of a âsyndemic.â
That, unfortunately, is a real word for a situation where two epidemics intersect, possibly making both of them worse.
COVID-19 is one of them, of course. The other is HIV/AIDS, which has claimed 32 million victims over the last four decades.
People with weakened immune systems are known to be more vulnerable to COVID-19. But thanks to antiviral medications, people who are HIV-positive can have healthy immune systems.
Indeed, over the course of the COVID-19 pandemic, there has been little evidence to suggest that people with HIV are more likely to become infected with the coronavirus â or that theyâre more likely to develop a serious case of COVID-19 if they do become infected.
But now researchers in South Africa have come across a patient whose HIV had not been well controlled with medication. The coronavirus seems to have had a field day with her, my colleague Melissa Healy reports.
The patient, a 36-year-old woman who was diagnosed with HIV back in 2006, contracted the coronavirus in September. She spent nine days in the hospital and was treated with supplementary oxygen, but she never became seriously ill with COVID-19.
Yet it took her immune system nearly eight months to shake her coronavirus infection. During that time, the virus underwent multiple genetic changes, some of them potentially dangerous.
The geneticists and infectious-disease specialists who cared for the patient suspect her uncontrolled HIV paved the way for her long-lasting coronavirus infection, which in turn gave the coronavirus ample opportunity to acquire mutations that could result in yet another variant of concern.
The researchers donât know whether any of the mutations detected in the South African patient wound up spreading to other people. But they said itâs probably not a coincidence that so many troubling variants have emerged in places like South Africaâs KwaZulu-Natal province, where more than 25% of adults have HIV.
Indeed, her case underscores a difficult truth: Rich nations like the U.S. can blanket their citizens with COVID-19 vaccines, but theyâll still be vulnerable as long as the coronavirus is spreading in other places where a lack of vaccine has kept immunization rates low.
Thatâs especially true in countries like South Africa, where HIV infections are common but often undetected.
âThis underscores the advantage that this virus has until we can put the brakes on it, and we have to put the brakes on it globally,â said Dr. Bruce Walker, founding director of the Ragon Institute, an immunology research center in Boston.
By the numbers
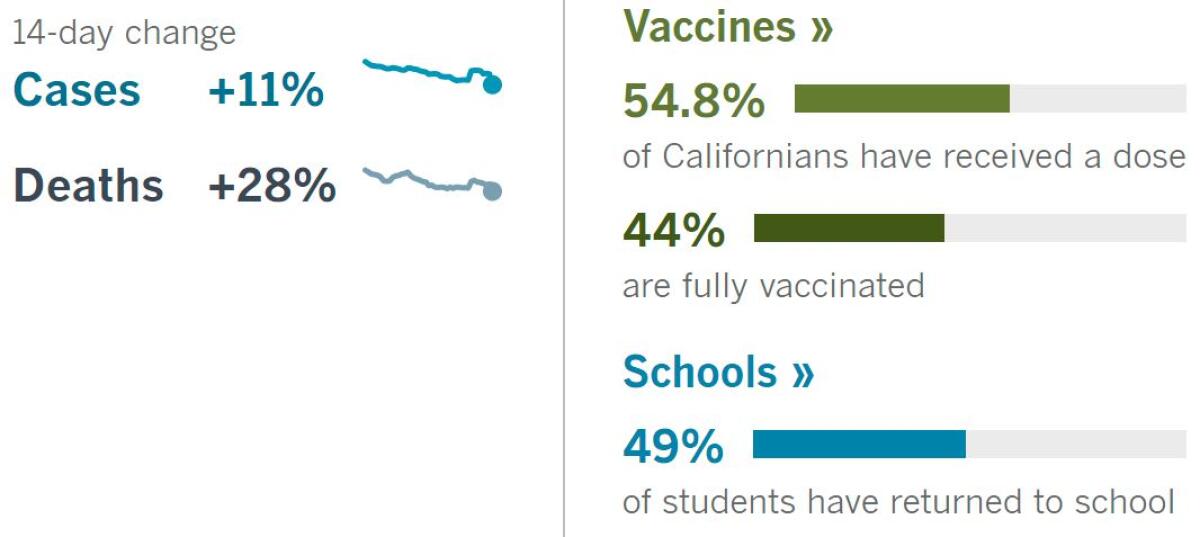
California cases, deaths and vaccinations as of 6:17 p.m. Thursday:

Track Californiaâs coronavirus spread and vaccination efforts â including the latest numbers and how they break down â with our graphics.
Across California
Going maskless at work? That may soon be possible for many vaccinated workers in California, after a state workplace safety board on Thursday evening recommended relaxing rules.
The board-approved proposal would let workers in a room take off their masks if everyone there is fully vaccinated and does not have COVID-19 symptoms. Masks would still be required if anyone present is not fully vaccinated or if anyoneâs vaccination status is unknown.
Restaurant and retail workers and others who interact with members of the public will probably still need to mask up for now. And in general, workers must be allowed to wear masks if they choose to do so, even if itâs not required.
The new rules are still subject to further review by the state Office of Administrative Law within 10 days.
During the pandemic, even while we were all in masks, all kinds of new communities were formed. My colleague Howard Blume brings us the story of one that came together as exasperated parents began to push for school to reopen and is now transforming itself into a nonprofit organization with a longer-term mission: inject parent power into a system dominated by teacher unions, administrators, school boards and state officials.
âParent voices and student interests should never again be ignored or deprioritized as they have been during this year,â said Megan Bacigalupi, the founder and executive director of the group. The pandemic has shown that the interests of parents and teachers unions donât always coincide, she said, and when they donât, parents need need a way to make themselves heard.
How powerful the group will become, and how representative it will prove to be, is of course yet to be determined. But parents will probably have a stronger voice in education politics than the powers that be have grown used to.
Pop-up restaurants are facing some political headwinds, too. When restaurants were forced to close and cooks and waitstaff found themselves out of work, these nimble food purveyors materialized all over Los Angeles. They operated out of homes and trucks and connected to customers through social media â some with permits, some not.
Now, with the state set for a full reopening June 15, the prospects for what writer Stephanie Breijo calls âsome of the most exciting dining the area has seen in yearsâ is uncertain. Many of the new businesses, serving fare as varied as cookies, cocktails and sambal goreng, plan to keep rolling; others will close as restaurant employees return to their regular jobs.
County health officials showed little inclination to enforce laws against âundergroundâ food operations at the height of the pandemic, but that could change. State law, meantime, could make things easier for small-scale food entrepreneurs.
There are two classes of legal âcottage foodâ operators. Class A operators can sell from their homes and at temporary events and farmerâs markets. Class B operators can sell to restaurants, stores and food trucks.
A bill that passed the Assembly last month would raise allowable revenue to $75,000 for Class A enterprises and $150,000 for those in Class B. A 2019 law allows for âmicroenterprise kitchen operationsâ to sell refrigerated foods, but issuing such permits is up to individual counties. Los Angeles County hasnât gotten around to it yet, though officials said that might happen in 2022. Some microenterprises could go out of business by then.
Brick-and-mortar restaurants and bars, meanwhile, just got a reprieve from Sacramento: In a boost for the struggling dining industry, the state is extending the ability of restaurants and bars to serve alcoholic drinks in outdoor dining areas, for delivery and to-go through the rest of the year, Gov. Gavin Newsom said Thursday.
He also said heâs hoping in the coming months to pursue state legislation that will make it easier for local governments to retain outdoor dining if they so choose as the pandemic recedes.
The news out of Sacramento was less sunny for healthcare workers who helped steer the state through the pandemic. California Assembly members declined Thursday to vote on legislation that would have awarded them âhero pay,â effectively killing the effort for the year.
The bill would have required hospitals, clinics and skilled nursing facilities to pay medical professionals $10,000, with smaller bonuses for those who work part time. The payments would have been made in four installments over the course of 2022 in hopes the cash would entice healthcare workers to remain in their jobs, said the billâs main proponent, the Service Employees International Union California. Hospitals fiercely opposed it for its estimated $7-billion price tag.
On a grander scale, the freedom to go to church will henceforth be considered equivalent to the freedom to shop at Costco, under a pair of legal settlements agreed to by the state of California this week.
Lawyers who challenged the stateâs coronavirus rules on behalf of churches will receive more than $2 million in fees from state coffers.
The issue, which had reached the Supreme Court, stems from Gov. Gavin Newsomâs decision to shut down church gatherings last year to slow the virusâ rapid spread. The settlement includes a permanent injunction in line with Supreme Court rulings that found restrictions on houses of worship cannot exceed those on retail businesses, attorney Paul Jonna said.
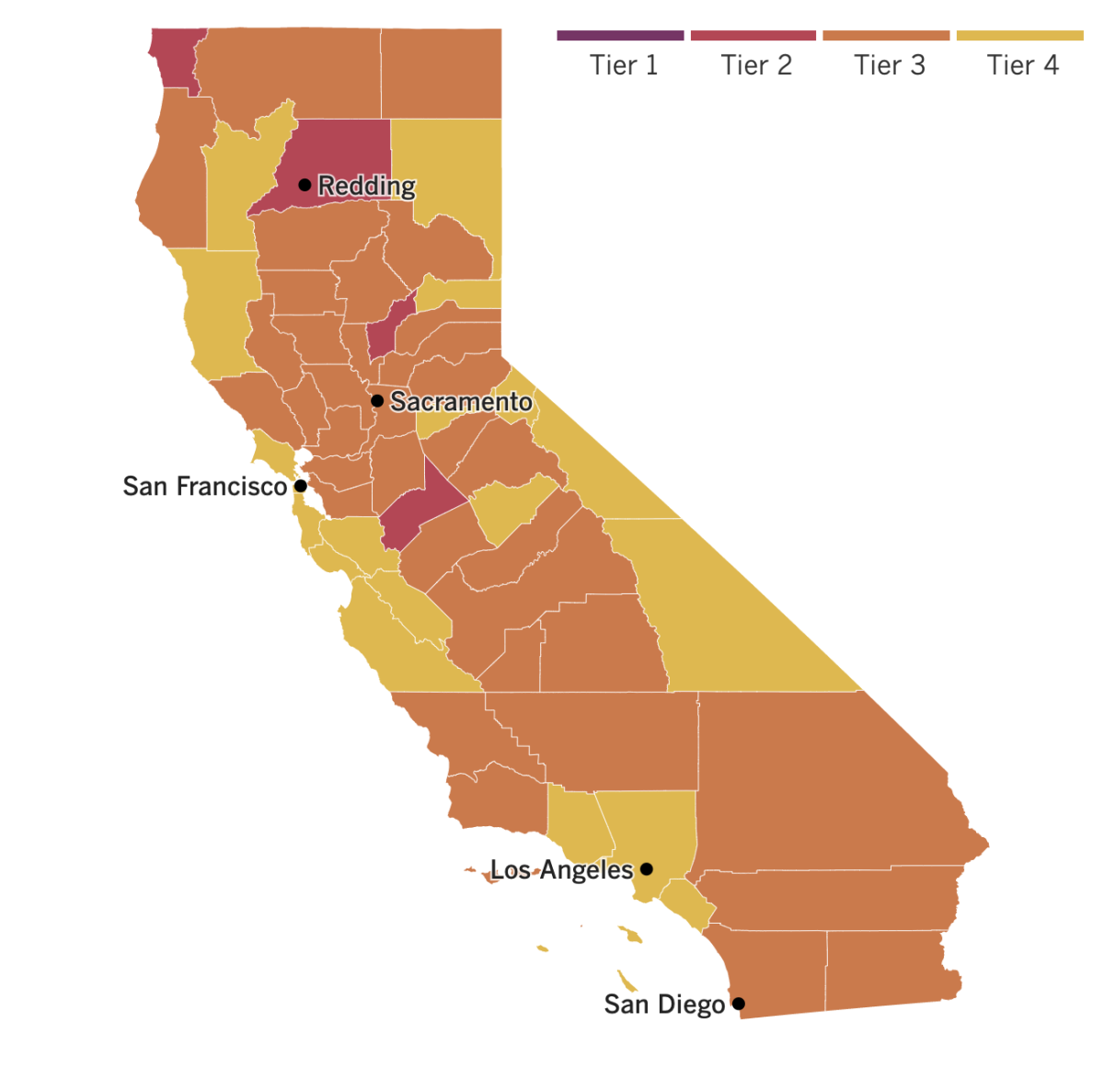

See the latest on Californiaâs coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
Just because millions of Americans canât be bothered to get vaccinated doesnât mean that COVID-19 vaccines should go to waste. President Biden said Thursday the U.S. will donate 75% of its unused vaccines to the United Nationsâ global vaccine-sharing program â with no strings attached.
âWeâre not seeking to extract concessions, weâre not extorting, weâre not imposing conditions the way that other countries who are providing doses are doing; weâre doing none of those things,â U.S. national security advisor Jake Sullivan said. âThese are doses that are being given, donated free and clear to these countries, for the sole purpose of improving the public health situation and helping end the pandemic.â
Still, the U.S. âwill retain a sayâ on where the vaccines go, he said.
The U.N. program, known as COVAX, has shared 76 million doses with needy countries to date. Of the nearly 19 million U.S. doses immediately headed for COVAX, about 6 million will go to South and Central America, 7 million to Asia, and 5 million to Africa.
The White House aims to share 80 million doses globally by the end of June, mostly through COVAX, but 25% of U.S. excess supply will be kept in reserve.
The shelf life of those vaccines, though, must be closely monitored. Some state officials in recent days have indicated that a portion of their unused doses may expire by the end of the month.
Vaccine expiration dates are based on a âpotency assayâ that can vary by vaccine. Some vaccines can last for two years or more if properly stored.
The COVID-19 vaccines authorized in the U.S. â made by Pfizer and BioNTech, Moderna and Johnson & Johnson â can last for up to about six months from the time of manufacture, depending on how theyâre stored. But because they are new, that amounts to a rough estimate.
COVID-19 vaccines remain stable longer at lower temperatures, which may be a problem when theyâre sent to areas that lack adequate refrigeration.
The troubled Tokyo Olympics caught another blow this week when it was revealed that about 10,000 of its 80,000 unpaid volunteers wonât participate when the Games open July 23.
Officials said theyâre not sure why. âWe have not confirmed the individualsâ reasons,â event organizers said in a prepared statement.
Fear of getting sick with a deadly disease, maybe?
Whatever their motivation for backing out, officials said the loss of volunteers would not affect operations of the Games, which had been postponed a year because of the COVID-19 pandemic.
The International Olympic Committee said it expects 80% of athletes and Olympic Village residents to be vaccinated. But anti-event sentiment is widespread in Japan, where only 2% to 3% of the population is fully vaccinated. Public opinion polls show 50% to 80% say the Games should not open, depending on how the question is asked.
The situation is bad in Japan, but itâs horrific in India, which is in the midst of its second COVID-19 surge.
Just how bad is it? No one really knows, especially in the countryside, where two-thirds of Indians live â often in deep poverty. âIt could be serious, very serious or disastrous,â said R. Ramakumar, a professor of development studies in Mumbai.
The official COVID-19 death count in one of Indiaâs poorest states, Uttar Pradesh, was 337,989 on Thursday, with 28 million infected. But a shortage of testing kits, a sorely inadequate health care infrastructure, and serious issues with government data collection and reporting mean the true figures could be up to five times higher, according to some experts.
That matters, because undercounting cases now could result in a false sense of security and heighten the risks of a third wave in the months ahead.
Indiaâs cities are hit hard, too, of course. But in the impoverished countryside, many people lack smartphones to receive basic information or communicate with healthcare workers. No Twitter access means less chance distant government officials could learn that oxygen tanks or hospital beds in a particular area are unavailable or in short supply.
Rural health system workers say itâs hard to provide even basic care without thermometers, devices to measure blood oxygen levels or other fundamental tools.
Patients seeking hospital care are trading in personal items and taking out loans to pay for it. A woman in the state of Maharashtra said she and her husband spent their annual income for treatment at a private hospital. Many others are unable to afford any kind of care.
Itâs all a harrowing manifestation of Indiaâs extreme levels of economic inequality.
Your questions answered
Todayâs question comes from readers who want to know: Can COVID-19 vaccines actually spread the coronavirus?
No. Social media is rife with false rumors, and the idea that COVID-19 vaccines can spread the coronavirus is one of them. Letâs be perfectly clear: There is no truth to this claim at all.
So where did it come from? Some people are spreading this lie on social media along with entreaties to send them money, said Barbara Ferrer, director of the Los Angeles County Department of Public Health.
âDonât get played by these people,â she said.
The COVID-19 vaccines available in the U.S. donât contain any part of the virus â âlive, dead, in parts or in whole,â Ferrer told The Times. âBecause of this, people who get vaccinated do not become infectedâ with the coronavirus, she said.
Possible vaccine side effects such as tiredness, headache, muscle pain and fever â which are generally mild and usually go away after a day or two â are not signs that youâve been infected with the virus. They are a response to the immune system gearing up to produce the antibodies you need to fight off the actual coronavirus. âThese side effects go away on their own, unlike COVID infection itself, which lasts often for a while and can cause very serious illness,â Ferrer said.
Moreover, since the vaccines donât contain any coronavirus, itâs impossible for the vaccine to make someone contagious.
But misinformation can be contagious, so do yourself â and the rest of us â a favor by not spreading it. If false rumors and outright lies cause too many people to avoid vaccination, it will take longer for the economy and life in general to get back to something close to normal.
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them. Wondering if your questionâs already been answered? Check out our archive here.
Resources
Need a vaccine? Sign up for email updates, and make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the stateâs COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get tested? Hereâs where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
Weâve answered hundreds of readersâ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




