Coronavirus Today: What Alaska can teach us about vaccination
Good evening. Iâm Thuc Nhi Nguyen, and itâs Thursday, March 18. Hereâs whatâs happening with the coronavirus in California and beyond.
In Alaska, where remote villages dot much of the wide, harsh terrain, getting a dose of COVID-19 vaccine may be easier than getting an Amazon package delivered to your door.
The state has become one of the countryâs leaders in vaccination rates by throwing out the eligibility rule book, my colleague Emily Baumgaertner reports. More than 29% of Alaskans have received at least one dose of a COVID-19 vaccine, according to data from the Centers for Disease Control and Prevention. (The national average is almost 23%.)
Last week, Alaska became the first state to make COVID-19 vaccines available to anyone 16 or older, as long as they live or work there. The decision was made after health officials realized their system suffered from paralysis by over-analysis. Too many residents were confused about whether they qualified, and too many appointments were going unclaimed â so the experts ditched their two dozen pages of eligibility restrictions.
âIt was astonishing to our team how much time and effort was being sucked up early on by constantly trying to make sure the right people got the vaccine, and nobody else,â said Tessa Walker Linderman, who co-leads Alaskaâs COVID-19 Vaccine Task Force. âOnce we decided to open up the gates, we were able to step back, breathe and think more strategically about how to fill in gaps.â
By contrast, Gov. Gavin Newsom calls equity the âNorth Starâ of Californiaâs vaccination effort. With essential workers putting their lives on the line and with Black and Latino communities disproportionately suffering, it seems like the right thing to do.
But executing it has been hard, with a state appointment system that doesnât allow local officials to set aside slots for specific groups. Recently, Pasadena canceled a clinic when too many ineligible line-cutters signed up for slots meant for people 65 or older and essential workers. Though Iâm personally frustrated by line-jumpers, I found myself wondering whether the goal of vaccinating everyone in just the right order could be doing more harm than good in that case.
The top-down bureaucratic approach is âone of the great ridiculous tragedies of this rollout,â said Arthur Caplan, a bioethicist at New York University. âWe are way too far into the swamp of dictating how to do this fairly, and itâs getting in the way of distribution.â
Alaska has some unique attributes. There are no county public health departments working alongside the state that could add more red tape to the process. Also, members of the stateâs 229 sovereign tribes are eligible for vaccinations through the federal Indian Health Service, and the stateâs large number of military veterans can turn to the Defense and Veterans Affairs departments.
Challenges presented by the stateâs natural environment are nothing new to Alaskan officials, who were ready to partner with tribal health systems and community clinics that already served the most vulnerable groups. For example, some Indigenous villages in the Aleutian Islands donât have running water but got vaccines delivered by door to door by healthcare workers on dog sled.
âEvery Alaskan community looks different,â said Dr. Anne Zink, the stateâs chief medical officer, âand when we brought their representatives to the table, it was clear they each needed a different approach.â
By the numbers
California cases, deaths and vaccinations as of 7:27 p.m. Thursday:

Track Californiaâs coronavirus spread and vaccination efforts â including the latest numbers and how they break down â with our graphics.
Across California
California doesnât have dog-sled delivery for vaccines, but it is making progress with its rollout.
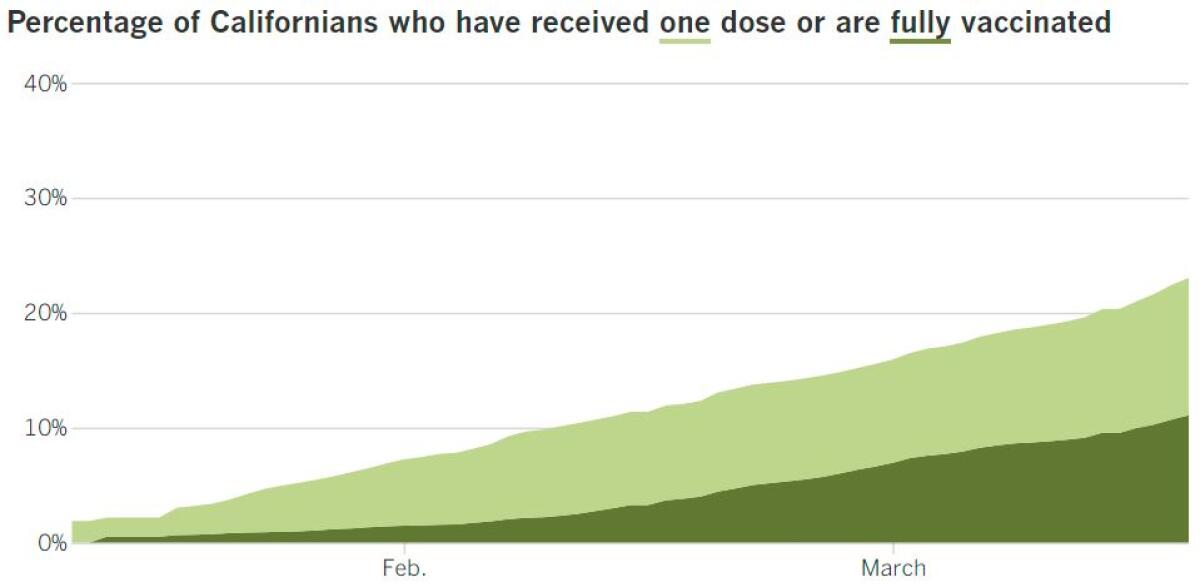
The last four days have seen the stateâs four highest single-day totals of vaccines administered, and nearly 1 million Californians have gotten a shot in the last two days, my colleagues Luke Money and Colleen Shalby report. Tuesdayâs 464,249 doses administered was an all-time high, followed by 400,4360 on Wednesday.
With about 23% of residents having received at least one dose of vaccine, California ranks 33rd out of all states and U.S. territories, according to data from the CDC.
To speed up the rollout, places like Disneyland were used as mass vaccination sites. Soon, however, it will reprise its role as the âHappiest Place on Earth.â The theme park in Anaheim will open April 30 â but the path back to business is difficult for the areaâs large amusement parks, my colleague Hugo MartĂn reports.
In addition to rehiring and training thousands of workers, Disney has to adopt new safety protocols that dramatically alter how dozens of attractions will operate and how visitors will be expected to behave. The state isnât making it any easier by not releasing detailed safety protocols yet.
So far, there are only a few marching orders from the state: All visitors must be California residents, and they all must wear masks. Indoor dining will be prohibited. Workers must undergo weekly coronavirus testing. Attendance will be capped at 15% for parks in red-tier counties (thatâs where Orange County is now), and individual indoor attractions will be limited to 15% capacity with time restrictions.
Some plans involve installing plexiglass barriers between parkgoers and employees, having limited seating on attractions and allowing a limited number of people to enter a line.
Disneyland without the lines sounds ideal, but be warned: Single-day ticket prices are expected to be in line with last yearâs prices. (The same is true for Universal Studios Hollywood, where attractions like motion-simulator rides wonât be open yet.)
A year since the pandemic first forced us to hunker down, Californians are not yet back to their B.C. (before coronavirus) rhythms, but weâre getting there, according to cellphone data collected by Google.
Following Californiaâs stay-at-home order in March, travel for work plummeted 51% by late April, and trips to retail stores and restaurants dropped as low as 55% below normal levels. Grocery shopping, which surged to 16% above the baseline in the immediate days after stay-at-home orders, dropped to 23% below baseline by April 13.
Now, travel for retail and restaurants is 26% below where it was before all of this craziness began, while grocery and pharmacy trips are 11% below. People have been slowest to return to work, which was at 33% below baseline.
Some experts are concerned that the longer we stay in our locked-down states, the harder it will be to emerge from them. One example is returning to public transportation. The people who are starting to move again are doing so primarily by car, a trend that could hurt public transit services â and the environment.
âThe longer the disruption is [and] the bigger the magnitude of the disruption, the higher the likelihood is that we might have bigger longer-term impacts,â said Giovanni Circella, a researcher at the UC Davis Institute of Transportation Studies.
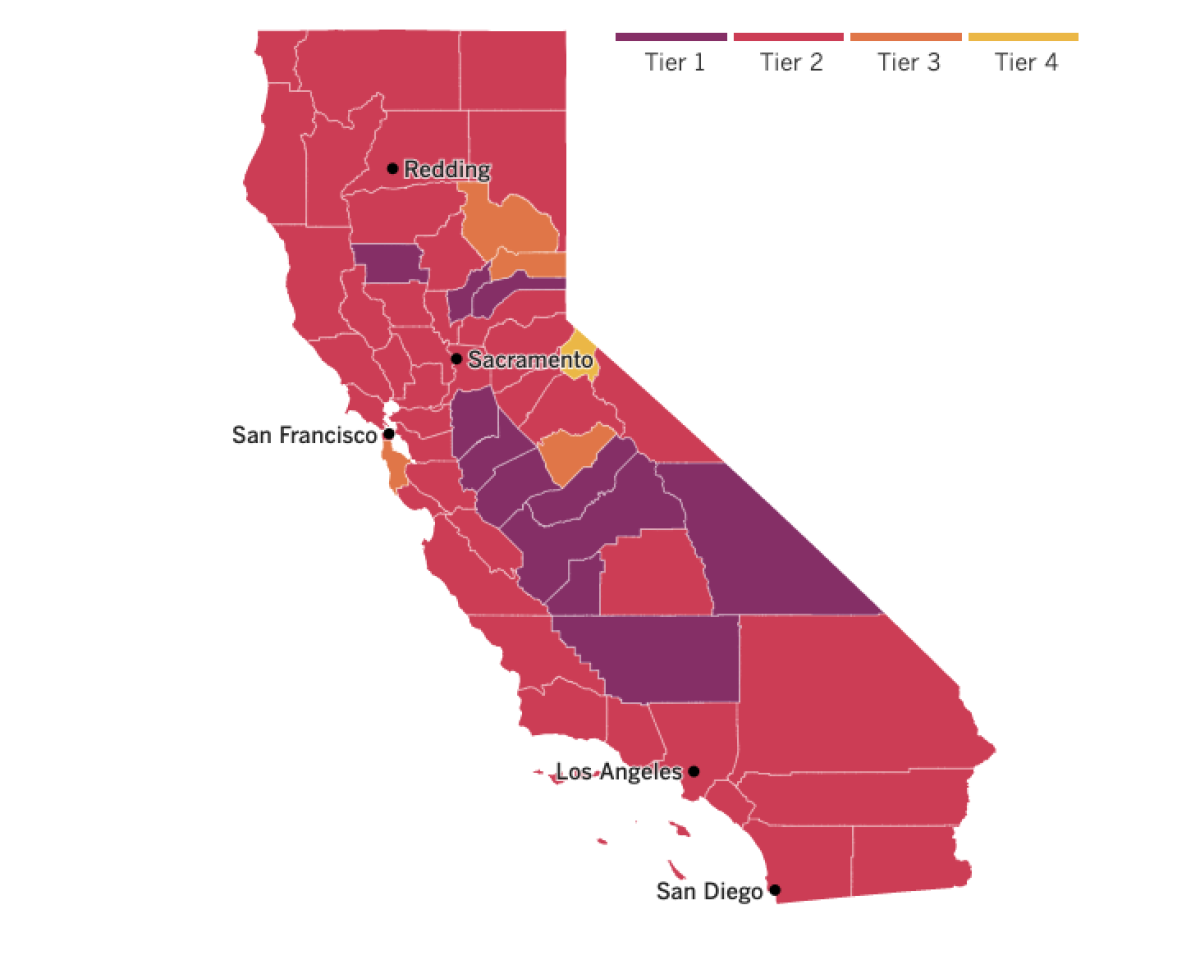

See the latest on Californiaâs coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
Like with Charles Darwinâs finches, the strongest coronaviruses will survive and thrive. Right now, the fight for variant supremacy in the U.S. centers on two main contenders, my colleague Melissa Healy reports.
Out of California is B.1.427/B.1.429, which accounted for 13% of all coronavirus samples that were genetically sequenced in late February as part of a new federal program. The competitor from the U.K., known as B.1.1.7, accounted for an additional 7% of the samples.
The Centers for Disease Control and Prevention declared the California strain a âvariant of concernâ this week. It is 20% more transmissible than its predecessors and is dominating in California, Nevada and Arizona. Like the U.K. strain, our homegrown variant seems to be less vulnerable to some medicines used to treat COVID-19. It has also shown signs of resistance to the current crop of COVID-19 vaccines.
But the U.K. variant has one key advantage: Itâs thought to be as much as 50% more transmissible than other variants. That edge could be all the strain needs to knock out any other challenger.
In a contest for population dominance, âspreading rules the roost,â said Dr. Eric Topol, director of the Scripps Research Translational Institute in La Jolla.
In January, CDC researchers projected that the U.K. variant would become the dominant strain in the U.S. by March, and epidemiologist Summer Galloway, the lead author of that report, said Wednesday that it probably accounts for 20% to 30% of the samples being sequenced today. Letâs hope both variants are knocked out sooner rather than later.
Dear reader, youâre probably reading this on a screen right now, and I encourage you to take a brief stretch break. We all need it.
As if the stress of the pandemic isnât back-breaking on its own, some of our work-from-home habits have left us suffering from musculoskeletal conditions such as achy necks and sore joints from hunching over our dining tables or sinking into beds that double as office chairs.
The work-from-home boom that has meant pain for many remote workers has brought profits to certain businesses, my colleague Andrea Chang reports.
Stocks for furniture stores specializing in ergonomic chairs and standing desks are soaring. Brands that sell pain management products like hand-held massage devices are flourishing, as are start-up companies that specialize in digital healthcare programs to help customers manage musculoskeletal problems.
Some businesses helped their employees transition into a home office by providing equipment. There are also simple ways to fight off the work-from-home wear and tear, like taking a five-second break to stretch every 15 to 20 minutes, said Scott Bautch, president of the American Chiropractic Assn.âs Council on Occupational Health.
In Europe, drug regulators are giving the the all-clear to the AstraZeneca vaccine after reports of blood clots caused some countries to suspend use of the shots last week. The European Medicines Agency declared Thursday that the vaccine is safe and effective, adding that the rewards of vaccination outweigh the small risks.
Emer Cooke, who leads the agency, said officials âcannot rule out definitively a linkâ between the rare types of blood clots and the vaccine. However, she said, âour scientific position is that this vaccine is a safe and effective option to protect citizens against COVID-19âŚ. If it were me, I would be vaccinated tomorrow.â
The EMA recommended adding a description of cases of blood clots to the vaccine leaflets so that health workers and patients would be aware of the risk.
Blood clots, which could be deadly if they travel to the heart, brain or lungs, have been reported in at least 37 people out of the 17 million who have received at least one dose of the AstraZeneca vaccine in Europe. At least four people died.
Your questions answered
Todayâs question comes from readers who want to know: What do we know about the coronavirus spreading among high school athletes?
This is surely one of the many questions on the minds of many athletes, parents and coaches as youth sports get going again in Southern California. Itâs why this spring promises to be a chaotic one â and our high school sports columnist Eric Sondheimer will be covering it all in our new newsletter, Prep Rally.
So what do we know about the spread? There are some examples of outbreaks tied to youth sports in other states, but that doesnât necessarily mean games and other competitions canât go on safely.
One example to learn from took place in Florida, where an unnamed county hosted at a wrestling tournament in December. One wrestler tested positive for the coronavirus after attending two tournaments. The county launched an investigation and identified 79 positive cases from 149 tests among a total of 576 people who attended the tournament or were deemed close contacts.
The outbreak resulted in the suspension of all winter indoor and outdoor sports for that county.
Now, time for context: At the time of the tournament, the county was in the CDCâs highest category for community transmission, with a test positivity rate of 7.7%, and the two-week cumulative incidence was 363 cases per 100,000 people. (Also, itâs impossible for athletes to maintain physical distance while competing in a wrestling match, and even the American Academy of Pediatrics says masks are ill-advised because they could present a choking hazard.)
The community infection rate is one of the top things to consider when deciding whether it is safe to let kids return to sports, said Dr. Matthew Mimiaga, a professor of epidemiology at the UCLA Fielding School of Public Health. Because California waited for cases and positivity rates to go down before allowing high school sports to resume, athletes here are probably at lower risk than those in Florida.
Officials in Minnesota are grappling with outbreaks linked to club sports like hockey, basketball and wrestling. Youth sports were paused in Carver County because many of the infections have been caused by the worrisome coronavirus variant from the U.K.
Despite alarm bells that may be going off at the mention of another shutdown, experts caution against blaming sports for viral transmission. Instead, the virus could be spreading in the course of socializing among teammates â for example, locker room chats, carpooling and team meals â rather than at practices or games.
Thatâs what researchers found when they studied 136 professional rugby players who participated in four Super League matches in Europe. Eight of the players tested positive for infections, and the researchers found that those cases were âmost likely traced to social interactions ⌠and not linked to in-match transmission.â Their findings were reported in the British Journal of Sports Medicine.
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them. Wondering if your questionâs already been answered? Check out our archive here.
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if youâre eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Need more vaccine help? Talk to your healthcare provider. Call the stateâs COVID-19 hotline at (833) 422-4255. And consult our county-by-county guides to getting vaccinated.
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get tested? Hereâs where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
Weâve answered hundreds of readersâ questions. Explore them in our archive here.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




