Coronavirus Today: How to vaccinate homeless Angelenos
Good evening. Iâm Thuc Nhi Nguyen, and itâs Wednesday, Feb. 17. Thank you to those who wrote emails and welcomed me to the newsletter after my debut yesterday. I appreciate your kind words as we continue this journey together. As a note for those wondering, my first name is actually Thuc Nhi, pronounced âToo-k Knee.â
With the extended introduction done, hereâs whatâs happening with the coronavirus in California and beyond.
Attempting to sign up for a COVID-19 vaccine has been, to put it plainly, a nightmare for many Angelenos. Phone lines are jammed, websites are crashing, and the number of appointments is extremely limited.
All of this is even more daunting for homeless Angelenos.
Consider Lance Curtis, a 65-year-old who lives in a single-room-occupancy building on skid row. When he saw Dodger Stadium turn into a vaccination site, he wondered how he would be able to get in line. He doesnât have a car.
Luckily for Curtis, doctors and nurses came to him.
Los Angeles Christian Health Centers and officials from the Los Angeles Department of Health Services are calling people in homeless shelters and setting up clinics near encampments to ensure this hard-to-reach â and especially vulnerable â group is protected.
But the effort to vaccinate the homeless population and skid row community is fraught with obstacles, my colleague Benjamin Oreskes writes. A transient population is, by its nature, a moving target. Physically delivering the vaccine is difficult: It has to be stored at freezing temperatures, canât be shaken, canât be in direct sunlight and must be used within hours of being defrosted. And on top of all this, many of the people health workers are trying to reach are suspicious of authority and, as a result, the need for vaccination.
Officials at Los Angeles Christian Health Centers receive about 100 doses per week to distribute across six clinics in L.A. County. The Department of Health Services adds about 400 to 500 doses per week for the homeless population. Itâs not even close to enough to protect the roughly 66,000 people in L.A. County who are homeless.
But for healthcare workers who treat homeless patients, itâs a welcome start.
Nurses and doctors try to focus on shelters and encampments that have suffered outbreaks, including one in Leimert Park. Officials knocked on RV doors and bent down to the pavement to speak to those who had been sleeping on the sidewalk. They assured people of the vaccineâs safety, observed patients for 15 minutes after receiving their shots in case they suffered allergic reactions, and offered food, clothes and juice.
Personal touches like these may be the key when it comes to vaccinating skeptical communities. Curtis, after speaking to nurses, personally convinced his friend and neighbor Cornelius Kincy to get the shot as well. They went together.
âThey told us weâre not going to die,â Kincy said. âWeâre not going to throw up. Weâre not going to get the runs.â
After their 15 minutes of observation and with the approval of nurses, Kincy and Curtis then went to the store for a celebratory beer.
By the numbers
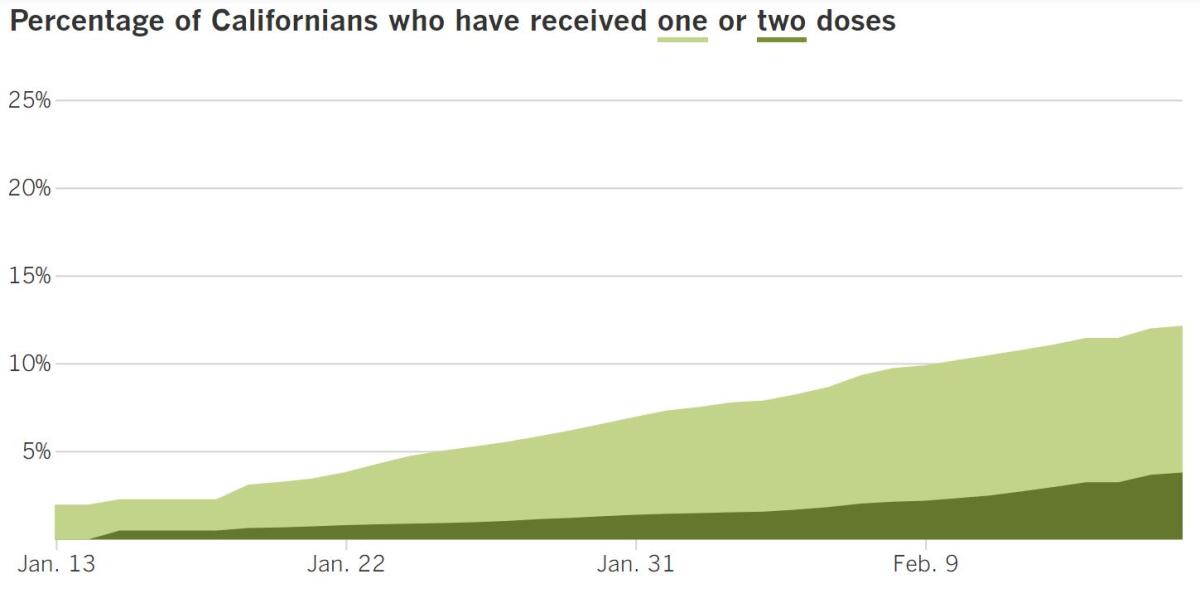
California cases, deaths and vaccinations as of 5:15 p.m.:

Track Californiaâs coronavirus spread and vaccination efforts â including the latest numbers and how they break down â with our graphics.
Across California
After a dire winter surge, the worst of Californiaâs coronavirus crisis seems to be behind us as cases have dropped to pre-Thanksgiving levels across the state.
Over the last week, California has reported an average of 8,087 new coronavirus cases per day. We havenât seen a number that low since mid-November.
The improving picture has made Gov. Gavin Newsom optimistic about the possibility of reopening more of the economy. Currently, 52 of Californiaâs 58 counties are in the most restrictive, purple tier, but Newsom said Tuesday he anticipates a âsubstantial numberâ of counties could move into the less restrictive red tier next week.
This week, Plumas became the latest county to advance to the red tier, joining Del Norte and Mariposa. Trinity, Sierra and Alpine are a step further, in the orange tier. No counties are in the most lenient, yellow category.
During the worst weeks of the winter surge, the state was reporting nearly 45,000 new cases a day, and the positivity rate for coronavirus tests was about 15%. Itâs fallen to 3.5% as of Tuesday.
The progress comes with a caveat: We didnât come this far just to come this far. Thereâs still work to be done as we wait for more vaccines. Newsom spoke at Cal State L.A. on Tuesday to inaugurate a new vaccination site there, and Orange County opened one at Santa Ana College on Wednesday to distribute vaccines to people 65 and older, healthcare workers and some law enforcement officers.
âWe do appreciate all the efforts everyone made to get us back to slowing the spread, and itâs our firmest hope that this continues,â said Los Angeles County Public Health Director Barbara Ferrer. âWe all have learned that this in large part depends on the actions of businesses and individuals as we wait for there to be enough vaccine doses for everyone in our communities.â
With case rates dropping, L.A. County allowed elementary schools to start reopening this week, but that doesnât mean all schools will be starting in-person classes immediately. The process will be uneven as circumstances vary between school districts.
My colleagues illustrated the discrepancies by introducing us to two families from nearby communities living in very different realities.
Stuart Waldman has two second-graders and one fourth-grader in Manhattan Beach and wants their schools to reopen fully soon. The district, which has a poverty rate of 5%, had already allowed students through second grade to come back to their campuses under a county-approved waiver.
On the other hand, Rogelio Rivas has two children in an Inglewood elementary school. Inglewood Unified has a poverty rate of 83%, and 71% of families surveyed there said they donât feel comfortable âsending their child back to school,â even if itâs allowed. Rivas joined the chorus.
âThe bottom line is Inglewood is mostly brown and Black kids whose parents are essential workers,â he said. âIf you send your kids into a school and they bring the virus back to your family where thereâs multiple generations living, itâs scary.â
Essential workers are among the first in line to receive vaccines to tame the pandemic, but the process to determine who is âessentialâ enough to receive a coveted shot has left millions of front-line workers in California without protection.
About 5.7 million people work on the front lines, doing things like packing food, pruning fields, cleaning offices and sewing cloth masks.
My colleagues Suhauna Hussain and Andrea Castillo spoke to Santiago Puac, who works in a clothing factory in downtown L.A. There are often 100 people from three different garment manufacturers packed into the same space. Even when Puac suffered body aches and lost his sense of smell, he continued to work because he couldnât afford to stay home.
At 42, Puac isnât old enough to qualify for the vaccine yet. His job isnât included in the current vaccination Phase 1B that covers essential workers in education, emergency services and food and agriculture. He believes some of his co-workers also went to work while sick because, like him, they needed to keep up with their finances.
Low-income Californians can expect some help in that regard, in the form of a one-time $600 stimulus check. Residents who have annual incomes of less than $30,000 and qualify for the 2020 California earned income tax credit are eligible for the stimulus checks, Newsom announced Wednesday. So are immigrants who are in the country illegally but who file tax forms.
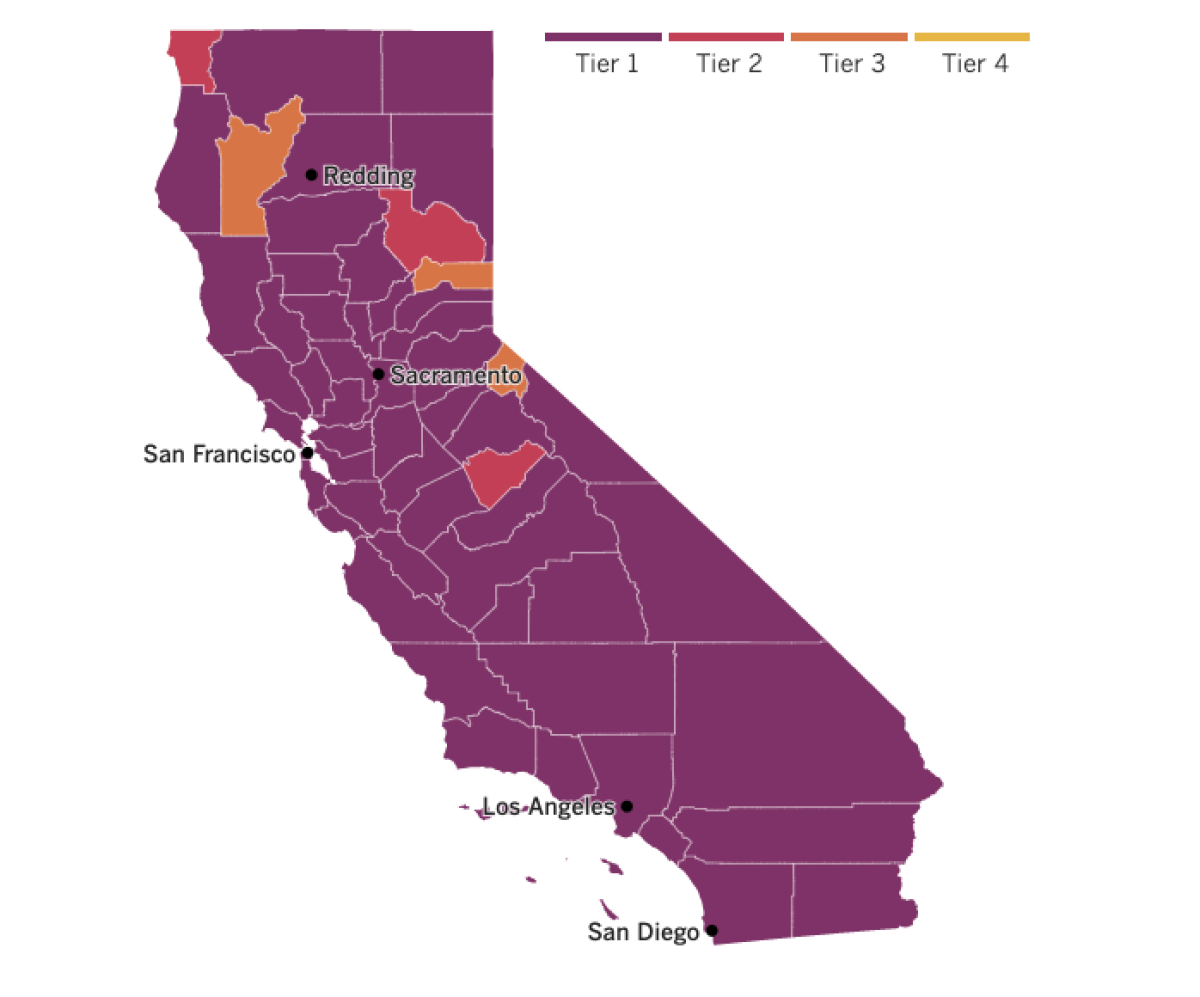

See the latest on Californiaâs coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
Part of the ânew normalâ has been finding novel ways to carry on old traditions. We had drive-through graduation ceremonies and Zoom Thanksgiving dinners. Theyâre decent substitutes for the time being, but nothing like the real thing.
Another iconic American celebration got a COVID-19 revamp as New Orleans hosted a quiet and cold Mardi Gras.
Bourbon Street was deserted amid coronavirus restrictions that closed bars and crowded streets. Instead of riding floats, some locals decorated their homes and tossed beads from their porches. Record-low temperatures added to the list of reasons to stay inside, where some would-be revelers settled for burning candles to honor the dead instead of leading processions.
Mardi Gras is often seen as a colorful, rowdy parade of people âhaving fun, doing their thing, parading, getting drunk or whatnot,â said 70-year-old Victor Harris. But it also has significant cultural meaning to local groups.
The cityâs Mardi Gras Indians, a tightknit group of Black working-class families, dress in flamboyant suits in honor of Native Americans who helped protect runaway slaves. They see the holiday as a time to connect with ancestors.
âGoing back all the way from slavery, itâs a spiritual thing for us,â said Harris, the big chief of the Spirit of Fi Yi Yi and Mandingo Warriors. âThis is the day to come together.â
With a subdued Mardi Gras in the books, President Biden remained cautiously optimistic that we could return to our old traditions soon with vaccination rates increasing.
The United Statesâ daily vaccination rate has almost doubled under Biden, going from about 900,000 per day during former President Trumpâs final full week in office to 1.7 million shots per day last week, according to data released by the Biden administration.
âBy next Christmas I think weâll be in a very different circumstance, God willing, than we are today,â Biden said during a CNN town hall Tuesday.
Supply problems continue to stifle the vaccination process, but Biden said he expected shots to be available for every American by the end of July.
Europe is also improving its vaccination effort. The European Union finalized an agreement with Pfizer and BioNTech to get 200 million more doses of their COVID-19 vaccine by the end of the year. Thatâs on top of an initial order of 300 million. About 75 million doses will be delivered between April and June.
Last month, Pfizer announced it was temporarily reducing deliveries to Europe and Canada while it upgraded production at its plant in Belgium. But BioNTech is starting production at a new plant in Germany this month.
While companies work to produce more doses to keep pace with the demand, scientists are monitoring the possibility of modifying their vaccine recipes so theyâre better equipped to deal with emerging coronavirus variants.
Weâve already seen more contagious strains, but scientists are wrestling with how to know when a variant has changed enough to warrant a booster shot or an entirely new vaccine. Some of the original COVID-19 vaccines are already proving to be less effective against the coronavirus strain from South Africa.
âWhen do you pull the trigger?â asked Norman Baylor, a former Food and Drug Administration vaccine chief.
Researchers are looking to the flu vaccine as a blueprint. Influenza mutates faster than the coronavirus, and modifying the vaccine every year is an international effort. National centers collect information about flu viruses on their turf and track their mutations before sending samples to World Health Organization-designated labs for more sophisticated testing. The WHO and regulators agree on each yearâs vaccine recipe before manufactures get to work.
Establishing a similar network of surveillance and testing for the coronavirus will be crucial to keep it at bay in the future.
Your questions answered
Todayâs question comes from readers who want to know: Should we be bracing for another surge in the spring?
This is an idea thatâs been making the rounds recently. Dr. Peter Hotez, an expert in vaccine development at Baylor College of Medicine and dean of the National School of Tropical Medicine there, is among those who say we should brace for a spike in cases in March and April.
âBeware of the Ides of March,â Hotez warned during this recent interview with the American Medical Assn.
But Dr. Anthony Fauci, the nationâs leading infectious-disease expert, has a different view.
âI do not believe that we should accept the inevitability of there being another surge,â he said on âL.A. Times Today.â âWe can prevent that by very carefully adhering to the public health measures that we speak about all the time.â
Those measures include universal masking, practicing physical distancing and resisting the urge to gather with people outside oneâs household, especially indoors.
These steps, combined with the stepped-up rollout of COVID-19 vaccines, should be enough to avert a spring surge, Fauci said: âIt could happen, but itâs within our power to prevent it.â
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them.
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if youâre eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get tested? Hereâs where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




