Coronavirus Today: These teens carry the world on their shoulders
Good evening. Iâm Amina Khan, and itâs Wednesday, Feb. 10. Hereâs whatâs happening with the coronavirus in California and beyond.
Iâve been thinking a lot about the stress and isolation the pandemic has caused so many students in the formative years of their lives and foundational years of their education. But I hadnât realized the extent of some teensâ burdens until I read Laura Newberryâs story about high school students who have taken up jobs and more family duties even as they struggle to keep up with their schoolwork.
Take 17-year-old Stephanie Contreras-Reyes, a senior at Orthopaedic Hospital Medical Magnet High School. Before COVID-19, she had a full plate: a slate of rigorous Advanced Placement classes, impressive extracurriculars, weekly volunteer work at two hospitals and plans to apply to Californiaâs top colleges.
Then the pandemic hit, and her dad lost his factory job. So she figured out how to sign her family up for food and rental assistance. She held garage sales on weekends and dropped off Tupperware catalogs to family friends. And then, when all of that wasnât enough, she took on shifts at the embroidery factory where her mom worked â all to help keep her struggling family afloat. âMy parentsâ worries became my own,â Stephanie said.
Stephanieâs AP U.S. History teacher, Heidi Mejia, says her student is remarkable.
A growing number of teenagers in Los Angeles have started working or taken on more hours for the sake of their families. They often carry overwhelming loads that can bring on anxiety attacks, depression and flagging grades. Mejia said about five students in each of her classes reach out daily to say theyâll miss school because theyâre working. âAnd those are just the students that are comfortable letting me know whatâs happening,â she said.
Across California, counselors are sending the same troubling dispatches. One described a senior at Oakland High School who, before starting to work full time this year, had a 3.9 grade-point average but is now failing almost all of her classes. A counselor at South L.A.âs Communication and Technology School worries about a student there who works from 4 p.m. to 4 a.m. five days a week and was so overwhelmed he tried to drop out â until the counselor dissuaded him.
Luis Leon can probably relate. Heâs a self-described average student at Woodrow Wilson High School and a happy-go-lucky kid with boundless energy in normal times. But between working 20 to 30 hours a week and watching his younger siblings, he was failing most of his classes by December. âMy friends have asked if I will drop out,â said Luis, who wants to study business and become a real estate agent. âBut I canât. I donât want my parents to see me that way. Iâll be their first son to finish high school. I want to go to college and make them proud.â
Rachel Varty, the college counselor at Stephanieâs high school, said students as young as 14 have been requesting work permits. Up north, a quarter of San Francisco International High Schoolâs 64 seniors are working 20 to 40 hours a week, said head counselor Oksana Florescu â more than double the usual number of working seniors. She coaches these students over Zoom on how to persuade their bosses to give them school-friendly schedules. âI give them talking points: âThis is my last year of school; Iâm trying to help my family,ââ Florescu said.
Antonio Roque, a counselor at Communication and Technology School, said the pandemic has thrown teenagers into the world of adult responsibility â and they are in survival mode. âTheyâre just doing what they need to do,â he said. âI think weâre going to start seeing the mental health consequences of this, the trauma, surface when schools reopen.â
Itâs an unbelievably high burden for students to shoulder, especially when their families â undocumented and first-generation Americans, essential workers and people of color â have already experienced more than their fair share of the pandemicâs punishments.
You should read this whole story. These students are inspiring; the troubles they face are appalling.
But Iâll leave you with this: Weâve talked a lot about getting kids back in school â and how that could help a lot of children who are struggling with social isolation as well as their academics. But a real-life classroom isnât going to help students who canât show up for class because they have a shift at their fast-food job or custodial gig, who are exposed to the coronavirus because they are front-line workers who donât have the option of working from home. Help for these students will require tackling the inequities that they and their entire families face, head on.
By the numbers
California cases, deaths and vaccinations as of 6:24 p.m. PST Wednesday:

Track Californiaâs coronavirus spread and vaccination efforts â including the latest numbers and how they break down â with our graphics.

Across California
Los Angeles health officials, facing a shortfall of COVID-19 vaccines, will close five city-run vaccination sites for at least two days beginning Friday, Mayor Eric Garcetti said Wednesday. He said the city had exhausted its supply of first doses of the Moderna vaccine and described the supply as uneven and unpredictable: This week the city received 16,000 doses. By comparison, it secured 90,000 doses last week and 29,000 the week before, he said. He said that anyone who has received a first dose of the Moderna vaccine will receive a second dose.
California has now racked up more COVID-19 deaths than any other state, my colleagues Luke Money and Rong-Gong Lin II report â a reflection of both its large population and a devastating holiday surge. More than 45,000 Californians have died of COVID-19, with 514 fatalities reported Tuesday alone, according to data compiled by The Times. That surpasses the 44,969 deaths in New York, which was crushed in the pandemicâs early days and became the poster child for how rapidly the virus could spin out of control.
The raw numbers are bleak, to be sure, but they donât tell the full story. When you consider that California is home to roughly 40 million people, the COVID-19 mortality rate comes out to 114 deaths per 100,000 residents â the 18th-lowest mortality rate among all states. For comparison, the corresponding mortality rate in Texas is 142 deaths per 100,000 residents, and itâs 135 per 100,000 in Florida. New Yorkâs is far higher, at 229 COVID-19 deaths per 100,000 residents, and the highest rate in the nation is in New Jersey, with 248 deaths per 100,000.
The latest surge is on the downswing, but more trouble may be on the way: The South Africa strain of the coronavirus has now been found in the Bay Area, Gov. Gavin Newsom said Wednesday, with one case in Alameda County and another in Santa Clara County. He did not share additional information on those who tested positive or how they may have contracted the variant. The news comes amid growing worries that a new crop of coronavirus variants, some of which are more contagious or more resistant to certain treatments, are on the rise in California.
Though currently available vaccines appear to be effective against most of the new variants, the one from South Africa, known as B.1.351, may be an exception. In a study involving a comparatively small group of about 2,000 people who were relatively young and healthy, the COVID-19 vaccine developed by AstraZeneca and Oxford University did not reduce the risk of mild to moderate illness. Another vaccine developed by Novavax also was found to be nearly 90% effective against all types of COVID-19 when tested in Britain, but only 49% effective in South Africa. A third from Johnson & Johnson that reduced the risk of moderate to severe cases of COVID-19 by 72% in clinical trial participants in the U.S. was only 57% effective in South Africa.
California has also confirmed 159 cases of the variant first identified in the United Kingdom, designated as B.1.1.7. That is of particular concern for health officials, as it is believed to be about 50% more transmissible than its predecessors. Los Angeles County Public Health Director Barbara Ferrer said itâs clear that a fair number of variants are circulating in L.A. County. âThe variants are concerning, because if we let our guard down, the more infectious strains can become dominant,â she said. âAnd that just makes it a lot easier for this virus to spread.â
The school reopening debate may soon be coming to a head: The coronavirus infection rate is dropping quickly enough that the county may be able to meet the state standard for reopening elementary schools as soon as next week, Ferrer told school leaders Tuesday. But she also predicted that teachers and other school staff would not begin to be eligible for vaccines for another few weeks â and completing that vaccination process would probably take months.
Indeed, some L.A. County teachers, food workers and first responders could start getting vaccinations in two to three weeks, Ferrer said â a major step for the region. But with supplies expected to remain tight and most L.A. County seniors still waiting for their shots, it will take time for large numbers of educators to get them. Details of how to expand vaccine eligibility to these groups are still being worked out, such as having schools offer their own vaccination clinics.
Meanwhile, the âimperfect convergenceâ of improving health conditions and slow-to-rollout vaccines could soon force officials to make a difficult choice, my colleague Howard Blume reports: Either open campuses when the state deems it safe enough, or wait for teachers and other staff to receive the COVID-19 immunizations many of them are demanding. Ferrer stressed that once health metrics are met, the county would not direct schools on reopening decisions â that would be left to local school leaders.
On their face, Ferrerâs statements appear to leave little hope for a full return to campus this school year if vaccines are required first. But she did include some wiggle room: It might be possible for districts to set up âclosed podsâ of smaller groups of employees targeted for vaccines, which could maximize reopenings for certain grades or selected schools. Also, while the current two-dose vaccination process requires five or six weeks to achieve full immunity, that timetable could speed up if a new one-dose vaccine by Johnson & Johnson is approved in the coming weeks, a development Ferrer noted in a presentation to the L.A. County Board of Supervisors.
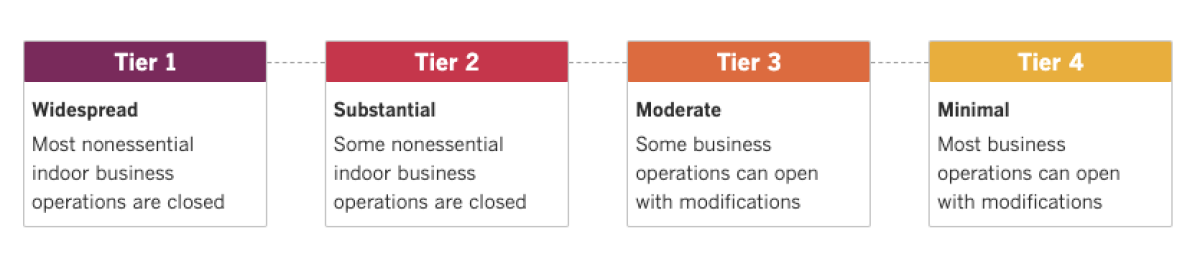
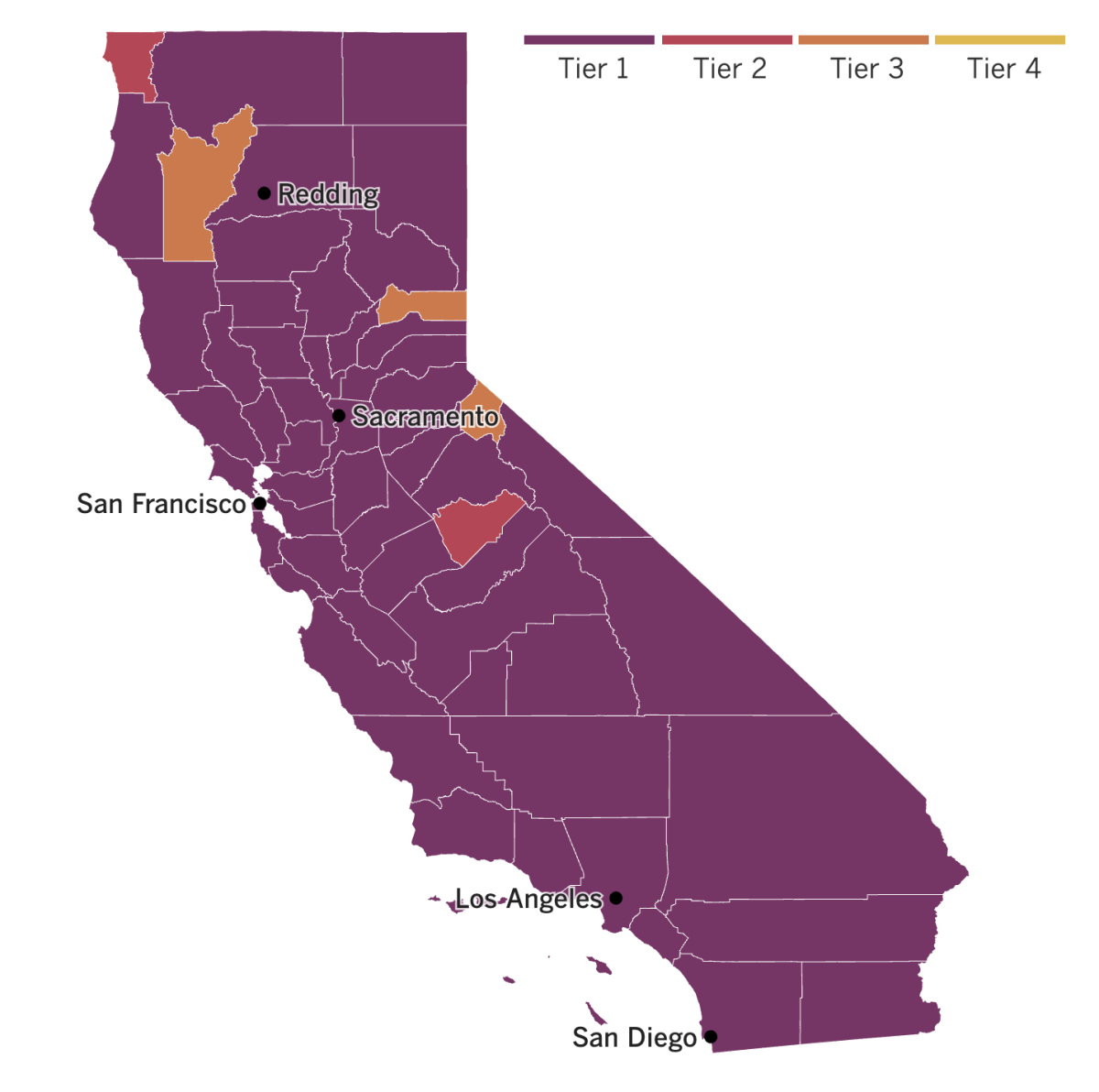
See the latest on Californiaâs coronavirus closures and reopenings, and the metrics that inform them, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
Well into the United Statesâ vaccination rollout, vaccine hesitancy remains worryingly high. Roughly 1 in 3 Americans say they definitely or probably wonât get a COVID-19 vaccine, according to the Associated Press-NORC Center for Public Affairs Research.
Thatâs a problem, because vaccines can stop community spread of a virus only once a large enough share of the population is inoculated. Two out of three people, or roughly 67%, wonât cut it. Dr. Anthony Fauci, the governmentâs top infectious-disease scientist, has estimated that somewhere between 70% and 85% of the U.S. population needs to get vaccinated to stop the scourge that has killed more than 470,000 Americans so far.
Though 13% of Americans have been vaccinated already and 54% say they âdefinitelyâ or âprobablyâ will get vaccinated, 15% are certain they wonât and 17% say probably not, according to the poll. Many expressed doubts about the vaccineâs safety and effectiveness â in spite of the fact that the vaccine drive has encountered very few serious side effects. Resistance appeared to run higher among younger people, people without college degrees, Black Americans and Republicans.
Older Americans, who are more vulnerable to COVID-19, were the most receptive to the vaccines: 20% of those 60 or older said theyâd already received a shot. Fifty percent of people in this age group said they would definitely get vaccinated, and 11% said they probably would.
An unprecedented string of federal executions at the end of the Trump administration at the United States Penitentiary at Terre Haute in Indiana probably acted as COVID-19 superspreader events, a new report finds. Some 70% of death row inmates were sick with the disease, as were guards and traveling prison staff on the execution team. So were media witnesses, who may have unknowingly infected others when they returned home because they were never told about the spreading cases.
Employees at the Indiana prison complex where the 13 executions were carried out over six months had contact with inmates and other infected people. Regardless, they were able to refuse testing and declined to participate in contact tracing efforts â and yet were still permitted to return to their work assignments. Other staff members, including those brought in to help with executions, shared tips with their colleagues about how they could avoid quarantines and skirt public health guidance from the federal government and Indiana health officials.
The last few executions completed in a short window over a few weeks probably fueled the virusâ spread, according to the records reviewed by the Associated Press. It was something health experts warned could happen when the Justice Department insisted on resuming executions during the pandemic. The Bureau of Prisons has repeatedly refused to say how many people have tested positive for the coronavirus after the last several executions. And the agency would not answer questions about the reason for withholding the information from the public. No more executions have been scheduled under Biden.
Now that South Africa has scrapped plans to use the AstraZeneca vaccine after some less than stellar results against the strain thatâs sweeping the country, officials instead will give the unapproved Johnson & Johnson vaccine to its front-line health workers beginning next week. The vaccination drive will double as a study to see what protection the J&J experimental shot provides against the variant dominant there, the health minister said Wednesday.
Zweli Mkhize said South Africa scrapped plans to use the Oxford-AstraZeneca vaccine because it âdoes not prevent mild to moderate diseaseâ caused by infections with the B.1.351 variant. The one-shot J&J vaccine has not yet been approved in any country. But Mkhize declared it safe in a nationally broadcast address, relying on test results of 44,000 people in South Africa, the United States and Latin America.
South Africa will also be using the COVID-19 vaccine made by Pfizer-BioNTech as well as others â possibly including the Russian Sputnik V, Chinese Sinopharm and U.S. Moderna vaccines, Mkhize said.
Your questions answered
Todayâs question comes from readers who want to know: Will wearing two masks protect me better than just one?
Thereâs growing evidence that the answer is yes. The latest data come from a report by the Centers for Disease Control and Prevention, which found that wearing a cloth mask over a tighter-fitting medical one decreased the wearerâs coronavirus exposure by about 95%.
The report has some caveats: Its takeaways are limited because the experiments âwere conducted with one type of medical procedure mask and one type of cloth maskâ and âdid not include any other combinations of masks, such as cloth over cloth, medical procedure mask over medical procedure mask, or medical procedure mask over cloth.â
But other experts have already been stepping in to provide detailed (and practical) guidance. Dr. Monica Gandhi, an infectious-disease specialist at UC San Francisco, co-wrote a commentary in the journal Med that drew upon principles from both infectious disease research and physical sciences to offer recommendations for masks.
She suggests double-masking for medically vulnerable people who are in high-transmission areas (including areas where new variants are circulating) when they have to go indoors (such as a grocery store). She also recommends it for others who may not be medically vulnerable but who do have to work in crowded, indoor conditions. But she doesnât advise double-masking for all people all the time.
As for what types of of double mask combos will work, you can wear a surgical mask and a cotton mask together (as the CDC recommends), or you could wear a cotton mask with a pocket for a filter between layers of cloth.
Gandhi does not recommend double-masking for children, for people in their late teens and early 20s, for people in areas with low levels of transmission, or for anyone when theyâre outside.
Wearing a mask is one of three basic preventive measures that can stop the coronavirusâ spread (the other two being physical distancing and good ventilation). If one of those three is compromised â say, if you have to go indoors â then you should bolster your protection from the other two (for example, by upping your mask game).
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them.
Resources
Need a vaccine? Keep in mind that supplies are limited, and getting one can be a challenge. Sign up for email updates, check your eligibility and, if youâre eligible, make an appointment where you live: City of Los Angeles | Los Angeles County | Kern County | Orange County | Riverside County | San Bernardino County | San Diego County | San Luis Obispo County | Santa Barbara County | Ventura County
Practice social distancing using these tips, and wear a mask or two.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get tested? Hereâs where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




