Coronavirus Today: This phone call could save lives
Good evening. Iâm Amina Khan, and itâs Wednesday, Dec. 2. Hereâs whatâs happening with the coronavirus in California and beyond.
At this point, youâre probably familiar with contact tracing â itâs how public health officials track and contain a disease outbreak. But what is it actually like to be a contact tracer in the midst of this fast-moving pandemic?
For Levonn Gardner, itâs an exercise in empathy and patience.
The Marine Corps veteran is one of those public health workers whose job is to notify people whoâve tested positive for a coronavirus infection and identify others who may have been exposed. Gardner said he gets a wide range of responses when he has to deliver the bad news: Iâm not surprised, or This is a hoax, or the heartbreaking I canât afford not to work.
Some of these conversations last minutes, while others go on for hours, my colleague Colleen Shalby writes. And much of the job depends on the intuition of the individual contact tracers, whose cultural backgrounds and appreciation for familial ties can make the task surprisingly personal.
âI understand hardship,â said Gardner, a Black man from Watts. âI understand what it means, especially, because it is primarily the Black and Latino communities that are dying from this and getting sick. Itâs people from my community.â
Contact tracing is a proven way of confronting outbreaks large and small. Thatâs why California has invested more than $27 million into these efforts, and why some 10,600 city, county and state employees have been deployed to track the coronavirus.
But the work requires cooperation on the part of the infected and the exposed. In mid-November, about 63% of people who tested positive in L.A. County and 71% of their contacts agreed to complete an interview. Many hang up, or argue that the virus isnât real.
For those who do stay on the phone, the anxiety is real â so having empathy for the people on the other end of the line is key. Roberto Melendrez, who has overseen a team of tracers in L.A. County for months, recalled conversations that left a lasting impression: The homeless man who said he couldnât afford to stop collecting recyclables, and the teenager who had become the caregiver for an infected parent.
âYou go through this very intense, intimate conversation with a group of people, and then you say goodbye,â Melendrez said.
In a time when so many of us canât interact with our loved ones except over the phone, I found the emotional moments these contact tracers shared with strangers to be truly heart-wrenching. Please read this excellent story.
And if you get a call that could be from a contact tracer, pick up the phone. It could save the life of someone you know.
By the numbers
California cases and deaths as of 4:46 p.m. PST Wednesday:

Track the latest numbers and how they break down in California with our graphics.
Across California
Both California and Los Angeles County are setting new records for coronavirus infections, hospitalizations and deaths almost every day. And thereâs no end in sight: The county is forecast to reach 9,000 cases by next week, county officials reportedly said.
The surge is putting pressure on public health leaders to take more aggressive steps to slow the virusâ spread. State officials have said they would consider a restrictive stay-at-home order if cases continued to rise, a scenario that increasingly seems all but inevitable.
Itâs possible that such an order would be imposed only on the worst-hit counties sitting in the most restrictive tier of the stateâs four-level pandemic reopening plan. Then again, most counties are in that tier, and together theyâre home to 99% of California residents.
A new lockdown order wouldnât necessarily be a repeat of the one in the spring. Thatâs because officials say they know more now than they did back then.
âOne of the most important things weâve learned is we can be not just more surgical with what we do, but we can really prescribe it for a shorter or a different amount of time,â said Dr. Mark Ghaly, Californiaâs health and human services secretary. âEarly on, some of those orders really were open-ended; we werenât sure. Today, we know that we can get impact from certain interventions in a reliable way more quickly, and thatâs part of what weâre considering.â
A big reason for considering a lockdown is the stateâs skyrocketing number of hospitalizations, particularly patients who require treatment in intensive care units. While ICU numbers havenât climbed quite as high as they did over the summer, theyâre getting closer by the day. As of Tuesday, there were 2,006 COVID-19 patients in intensive care â up roughly 75% from two weeks ago, and just shy of the stateâs all-time record of 2,058, set on July 21.
With the number of patients rising so fast, demand for these hospital beds could quickly outstrip the supply.
âWhat matters is a hospitalâs practical ability to take care of the patients that come in the door, and that requires not just a bed but, more importantly, it requires people, it requires staff, it requires supplies and equipment,â said Dr. Christina Ghaly, L.A. Countyâs director of health services.
San Francisco, once a shining success story, is poised to announce more rollbacks to its reopening plan, including a possible quarantine order for travelers and reduced indoor capacity at businesses.
Dr. Grant Colfax, San Franciscoâs director of public health, said shutdowns during the past few weeks have failed to stem the spread of infections. As a result, the city may be facing a shortage of hospital beds by Christmas. âWe know, unfortunately, that the worst is likely yet to come,â Colfax said.
Not every California community is on board. In Beverly Hills, the City Council unanimously voted to oppose L.A. Countyâs outdoor dining ban despite the unprecedented surge in cases. Council members cited the detrimental impact on local businesses and argued that there was a lack of scientific evidence to support the ban.
And fed-up protesters have gathered outside the homes of L.A. County Public Health Director Barbara Ferrer and L.A. County Supervisor Sheila Kuehl. Though both demonstrations were small, they were attended by mostly unmasked people and reflect a growing political divide over the pandemic health restrictions.
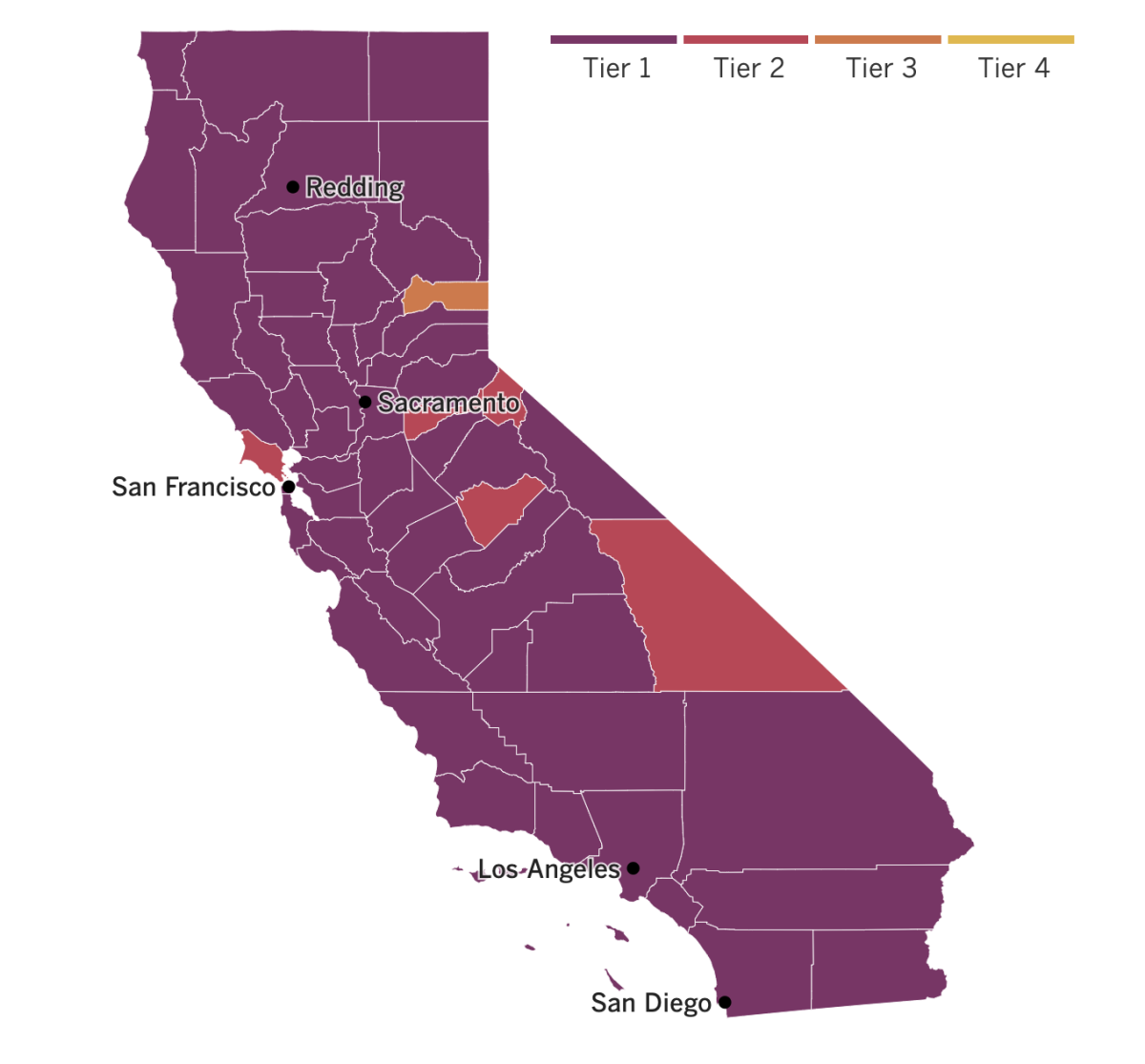

See the current status of Californiaâs reopening, county by county, with our tracker.
Consider subscribing to the Los Angeles Times
Your support helps us deliver the news that matters most. Become a subscriber.
Around the nation and the world
Some possibly good news for people who have been exposed to the virus: The Centers for Disease Control and Prevention have trimmed the recommended quarantine for anyone exposed to an infected person to 10 days, shaving four whole days off its previous advice. And if a person gets a coronavirus test three to five days after exposure and tests negative, they can resume normal activities after an even shorter period of seven days.
Hereâs the thing: The virusâ behavior hasnât changed. The incubation period for the coronavirus can extend to 14 days or even longer. But most infected people become infectious and develop symptoms between four and five days after exposure.
While allowing people to reduce the length of their quarantine does pose a small risk, the CDC said the change makes it easier for people to actually follow the agencyâs guidance.
The decision was based on extensive modeling, said Dr. John Brooks, chief medical officer for the CDCâs COVID-19 response program, and had been under discussion for some time.
In Nevada, Dr. Jacob Keeperman took to Twitter to post a selfie while wearing a face shield and personal protective equipment at a hospitalâs alternative care site. His goal was to drive home the seriousness of the pandemic.
Then conspiracy theorists picked up the photo and misrepresented it to spread the false notion that the pandemic was a hoax â even as cases continue to surge in the state.
Keepermanâs photo shows him standing in front of empty hospital beds and medical equipment set up inside a Reno parking structure to accommodate an overflow of COVID-19 cases if needed. Keeperman took the photo on the day the site was opened, before patients began arriving. But some on social media ignored that context, claiming that because the garage was empty, the pandemic was a âscam.â
According to Renown Regional Medical Center, which opened the alternative care site, the facility currently has 42 patients and has served 198 since it opened on Nov. 12.
âIt is really demoralizing to everybody who is out working so hard to have this politicized and polarized so much,â said Keeperman, who is medical director for Renownâs Transfer and Operations Center. âI am holding patientsâ hands when they take their very last breath because their loved ones canât be with them.â

Britain has now become the first country to authorize a COVID-19 vaccine following large-scale clinical trials. Regulators gave the shot developed by Pfizer and Germanyâs BioNTech the go-ahead for emergency use on Wednesday. Doses of the vaccine will be delivered to the country in the âcoming days,â officials said.
The vaccine is still under review by regulators in the U.S. and the European Union; a decision from the U.S. Food and Drug Administration on whether to authorize its emergency use is expected in mid-December. China and Russia have approved COVID-19 vaccines for early or limited use, but both countries issued the authorizations without waiting for the results of Phase 3 clinical trials.
Your questions answered
Todayâs question comes from a reader who wants to know: Is it safe to eat prepared foods that canât be cooked?
What this reader said she had in mind were items like coffee from a coffeeshop, salad from a restaurant and cupcakes from a bakery. She has avoided such foods out of fear that an asymptomatic food handler may have coughed or breathed on them, or their containers.
Donald Schaffner, a food microbiologist at Rutgers University, says the risks in these types of situations are âvery, very low.â
âWe have no documented cases of COVID-19 arising from food or from food packaging materials,â he explained. âThere are some papers coming out of China that do allege illness from food packaging materials, but I do not believe the science is solid enough to conclude that this is a risk that [is] reasonably likely to occur.â
The risk of getting the coronavirus from fomites â or inanimate objects which might carry infectious particles â is also quite low, and the number of documented cases is âexceedingly small,â he added. Most cases appear to come from close contact with infected individuals and from breathing in droplets or aerosol particles containing the virus.
âI think itâs important to realize that the overwhelming risk which comes from acquiring a cup of coffee or a cupcake will be the people you interact with in acquiring that food or beverage, i.e. other people in the store, the person serving you at the cash register, etc.,â Schaffner said.
âI recommend that in these situations people wear a mask and also practice as much physical distancing as possible within the store,â he added. âI do not advise consuming food or beverage while unmasked within a store. Wait until you are outside and away from other people before enjoying!â
We want to hear from you. Email us your coronavirus questions, and weâll do our best to answer them.
Resources
Practice social distancing using these tips, and wear a mask. Hereâs how to do it right.
Watch for symptoms such as fever, cough, shortness of breath, chills, shaking with chills, muscle pain, headache, sore throat and loss of taste or smell. Hereâs what to look for and when.
Need to get tested? Hereâs where you can in L.A. County and around California.
Americans are hurting in many ways. We have advice for helping kids cope, resources for people experiencing domestic abuse and a newsletter to help you make ends meet.
For our most up-to-date coverage, visit our homepage and our Health section, get our breaking news alerts, and follow us on Twitter and Instagram.




