Opinion: California’s great strides in Medi-Cal expansion are threatened by system inefficiencies
- Share via
California is striving for a healthier 2024 by vastly expanding its Medicaid program, but the state is at risk of rescinding coverage at the same time. Some of the sharpest impacts, both positive and negative, are affecting Latino health.
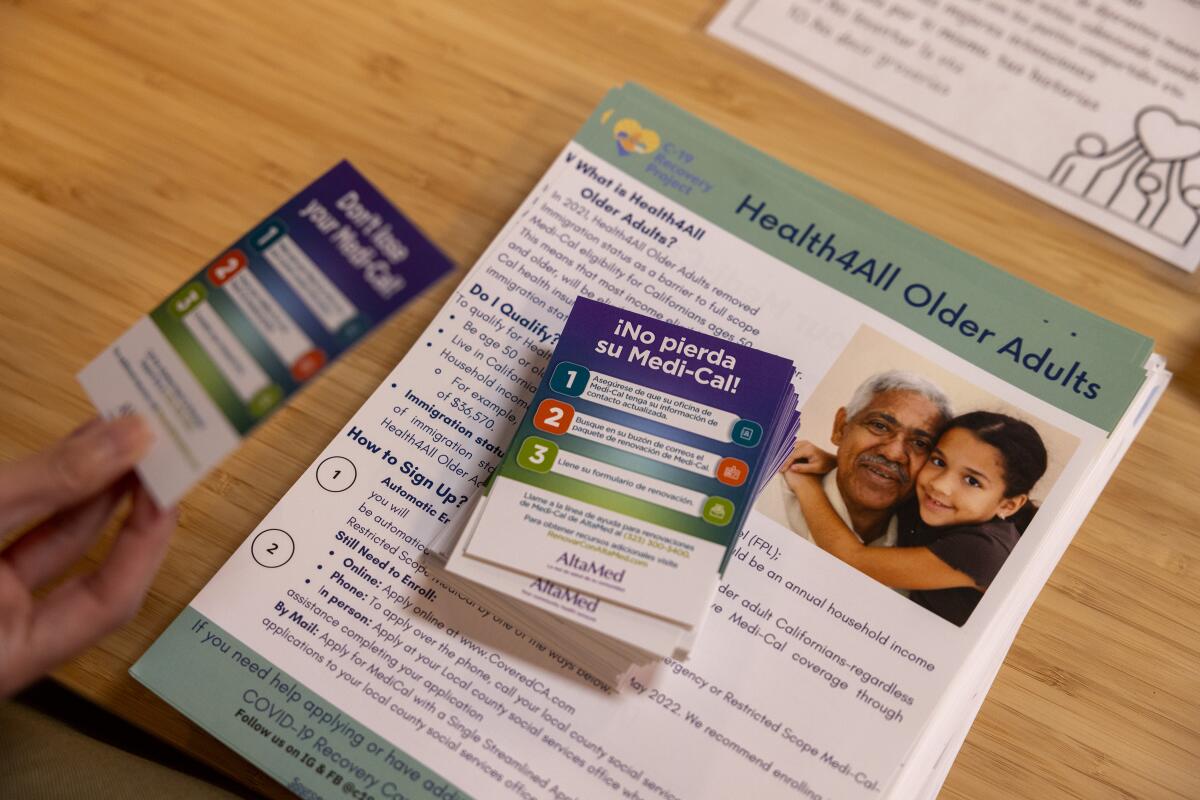
The expanded Medi-Cal aims to ensure that all California residents — regardless of citizenship — have access to life-saving care. This transformation leads us one step closer to universal coverage. Unfortunately, the great strides are being threatened by the annual Medi-Cal redetermination process.
Access to healthcare is more important than ever, especially for Latinos. Our community continues to suffer the acute effects of the COVID-19 pandemic as well as chronic conditions resulting from decades-long systemic disenfranchisement.
Next year, California will extend Medi-Cal benefits to the last group of undocumented people who have been left out of the program — those ages 26 to 49 — in what is expected to be its biggest expansion of coverage since the rollout of the Affordable Care Act.
California’s Medi-Cal system covers about 15.28 million people, and over 50% of those enrolled are Latino. Nearly a decade ago, our communities came together to build the framework to expand access to the state’s healthcare coverage to all Californians regardless of immigration status.
Today, anyone who is eligible for full-scope Medi-Cal will have the ability to apply for the benefit. It is a powerful legacy for Gov. Gavin Newsom and a huge victory for healthcare justice. But simultaneous Medi-Cal expansion and loss of coverage due to Medi-Cal redetermination — the annual verification of eligibility — puts us at a critical intersection.
At the start of the pandemic, Congress acted to ensure Medicaid recipients kept their benefits without the annual income and eligibility verification process. This was an intentional public health policy decision to ensure people didn’t lose their healthcare coverage when they needed it most. But when Congress uncoupled Medicaid’s continuous coverage from the official federal health emergency last year, the annual redetermination checks began again, sharply focused on income eligibility. Currently, the annual income requirement for a family of four to qualify for Medi-Cal is $41,400. Just a dollar over the threshold can make you ineligible.
The tentative figures are an early sign of the serious shift underway as the federal government has rolled back rules that helped people stay on Medicaid.
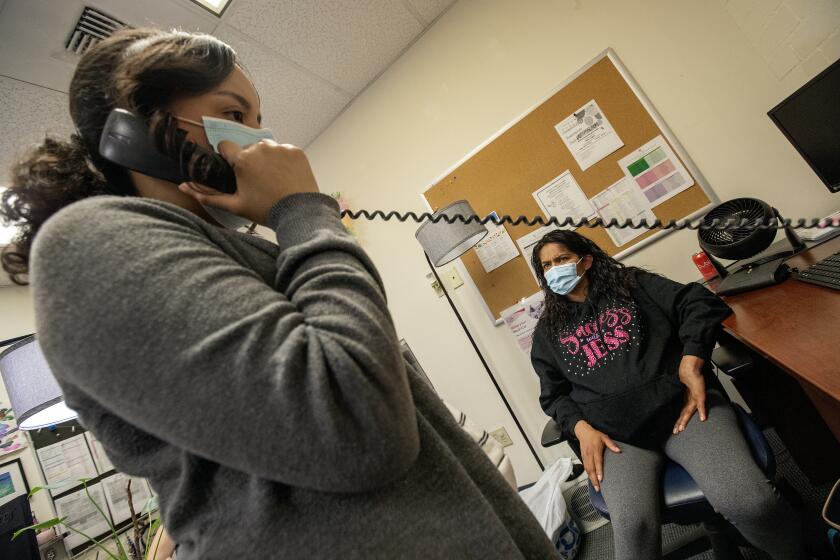
California began its Medi-Cal redetermination process in spring 2023. If the state’s systems can verify all of a member’s financial information, redetermination is automatic. However, early data show a troubling fact. From June through October of last year, just over 50% of all people disenrolled from Medi-Cal were Latino. These disenrollments were overwhelmingly due to procedural reasons, such as missing or incomplete paperwork, rather than reasons of eligibility.
Redetermination in Latino communities has been met with confusion and has taken people by surprise. Obstacles such as long work hours, access to transportation, language barriers and literacy all hinder our communities when they engage with formal systems, including healthcare. These disenrollments undermine California’s Medi-Cal expansion efforts and threaten the already fragile health of Latinos, 40% of the state’s population.
There are a few key actions California can take to address this issue. The state can pause procedural terminations so people don’t lose coverage because of a paperwork or process issue. Last fall, the federal government ordered 30 states to pause their redetermination efforts because of system errors in eligibility checks. This shows that pauses can be enacted to prevent incorrect disenrollments in 2024, and may even be possible to execute before the 2023 redetermination process ends in June.
California can also update the CalSAWS/BenefitsCal system to ensure there are expanded ways to check income eligibility, track information and communicate with users. California can also protect and increase the funds that go to community health navigators and organizations that work within the community to support enrollment efforts.
Despite a significant budget deficit, Newsom has shown himself to be a steadfast supporter of healthcare. Under his leadership, we are closing the Medi-Cal gap and moving a step closer to universal coverage. California is advancing health justice, and we cannot let confusing and inefficient redetermination processes undermine that effort. Progress can only be truly celebrated if we ensure accessibility within every corner of our state’s Medi-Cal program. The good news is, it’s not too late.
Seciah Aquino is executive director of Latino Coalition for a Healthy California, where Rita Medina is deputy director.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.