Op-Ed: The ‘deaths of despair’ narrative focused on white men. Whom did it leave out?

- Share via
In 2015, two economists introduced a social theory that would become one of the most famous of the era: deaths of despair. They speculated that rising rates of deaths among white Americans shared a common cause: rising despair and unemployment in areas such as the Rust Belt.
The theory immediately caught on in the public consciousness. It drew from data showing that premature mortality — deaths among 45- to 54-year-olds — was increasing, but only for white Americans. Data from Hispanic and Black Americans showed declining premature death rates, as did records from other affluent countries.
Adherents to this theory sounded the alarm: White people were dying at unprecedented rates — killing themselves, quickly or slowly — from drugs, alcohol and suicide, causes of death shown to be spiking for this demographic between 1999 and 2013.
U.S. life expectancy, already declining since the onset of the pandemic, fell further in 2021, according to the CDC’s final accounting of death certificates.
Mass media were captivated by the finding that white midlife mortality increased, treating it as more newsworthy than the routine reality that other groups — most conspicuously Black Americans — were still dying at much higher rates. As the deaths of despair framing gained ground, health equity scholars raised questions about the theory’s framing. The 9% documented increase in premature deaths among white people did not come close to catching up to the mortality rate among Black Americans; we found that to reach parity, the rate would have had to increase by more than 50%.
Now, nearly a decade after the phrase was coined, another flaw in this public health concept has emerged. That midlife deaths were increasing only among white people — particularly men without college degrees — was the core insight highlighted from the theory. But a new analysis shows that notion was never quite true.
In a recently published article in the Lancet, we provide new data showing that between 1999 and 2013, premature deaths among Native Americans increased by a far greater margin: nearly 30%. These deaths started at a much higher rate to begin with, and unfortunately the inequities have only deepened in recent years. We found that as of 2020, Native Americans had a premature death rate double that of white Americans. A disparity of this magnitude between ethnoracial groups should be inconceivable in our society.
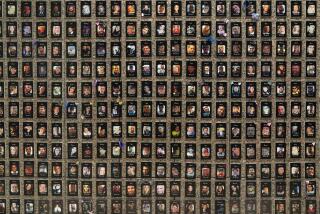
The case that white suffering was unique depended on the exclusion of data representing Native Americans. We call this practice “data genocide,” a term used by researchers at the Urban Indian Health Institute and other organizations. This concept recognizes that overlooking — or erasing — information about the disproportionate suffering of Native Americans is a long, commonplace tradition in this country, dating back to the days of ethnic cleansing and genocide against Indigenous people.
Data genocide includes practices such as simply not reporting data for Indigenous peoples, hiding them in an “other” or “multiracial” category, failing to posthumously identify individuals who identified as Indigenous while alive, or having insufficient outreach, trust-building and Native leadership input to ensure accurate data collection.
As the pandemic ravaged the country, deaths from drug overdoses surged by nearly 30%. The death rate was highest among Native Americans.
The increasing mortality rates among white Americans — especially those without a college degree — are troubling to be sure. That U.S. life expectancy has been declining since 2014 after decades of progress is cause for concern. But the narrative that white people were experiencing new, unique levels of suffering and despair obfuscated an inconvenient fact: As our research shows, midlife mortality is still significantly lower for white Americans than for Black and Native Americans.
The problem with focusing on despair in any racial group is that it emphasizes individual sufferers instead of a system that capitalizes on inequities. There are well-known, solvable reasons that the United States is an extreme outlier on the global stage when it comes to premature death.
When compared with some similarly wealthy countries, Americans die prematurely more than twice as often. This is no coincidence. It’s baked into the DNA of our country — starting with our violent past that has condemned generations of people to health struggles and economic precarity, and extending today to our profit-driven healthcare system and threadbare social safety net that help fuel our epidemic of early death.
The very structure of our country promotes despair in many of its people. We need progress on these issues to extend the lives of all Americans, and possibly reverse our unprecedented declines in life expectancy.
To combat the uniquely high premature death rates among Indigenous peoples, resources must be invested in a culturally appropriate way, controlled by tribes themselves, to improve access to employment, housing, substance use treatment and healthcare. These steps would at least bring us closer to racial equity — an imperative for the health of the nation and all its inhabitants.
Joseph Friedman is a researcher at UCLA who studies social inequalities and the overdose crisis. Helena Hansen is a professor, anthropologist and addiction psychiatrist at UCLA who researches race and addiction. Joseph P. Gone is a citizen of the Aaniiih-Gros Ventre Tribal Nation of Montana and a professor, psychologist and researcher at Harvard University, where he directs the Harvard University Native American Program.
More to Read
A cure for the common opinion
Get thought-provoking perspectives with our weekly newsletter.
You may occasionally receive promotional content from the Los Angeles Times.