End of an era: L.A. County lifts COVID-19 emergency

Los Angeles County is officially ending its COVID-19 emergency declaration Friday, a milestone that comes as the regionâs coronavirus case rate has fallen to its lowest level since summer 2021.
Itâs perhaps fitting that the nationâs most populous county delayed lifting its local declaration, doing so a month after the state. L.A. County has been one of the hardest-hit parts of California â so much so that the National Guard had to transport corpses from overwhelmed hospital morgues during the pandemicâs first winter. Officials also led the nation in sounding the alarm about the danger posed by the Delta variant, which fueled a significant surge the following summer.
But L.A. County health officials, like their counterparts across the state, say the local declaration has served its purpose and the region is now ready to enter a promising new phase.
âWhile it remains critical to continue to control the spread of COVID-19 in our homes, workplaces and communities, we no longer need to rely on emergency orders to ensure we have and can use life-saving tools and mitigation strategies,â Public Health Director Barbara Ferrer said this month. âInvestments made to date have resulted in robust tracking methods, ample testing capacity and effective vaccines and therapeutics.â
Los Angeles County will end its COVID emergency declaration at the end of March, becoming the latest region to do so amid improving pandemic conditions.
For much of the public, there will be few immediate changes. The county Department of Public Health will continue to provide free COVID-19 vaccines, tests and therapeutics.
The countyâs most visible health mandate â a universal mask order in indoor public settings â was lifted 13 months ago. And a recommendation for face coverings for the general public ended two months ago.
The pandemic saga is still being written, however. And its potency, though dulled, has not been dispelled.
âWe have to remain vigilant,â said Maria Van Kerkhove, the World Health Organizationâs technical lead on COVID-19. âOn the one hand, weâre in a much better situation. On the other, we canât predict with absolute certainty how this pandemic will unfold, with the exception that this virus is here to stay.â
But just as March 2020 is now indelibly etched in our collective consciousness â a watershed moment when daily life screeched to a halt â March 2023 may be remembered as when COVID-19 officially went from top of mind to back of mind.
In order to move through a world where the coronavirus is endemic, we need a reliable way to assess our individual level of immunity. Hereâs how we can.
One change that goes into effect Monday is the end â both in L.A. County and across California â of the government-ordered COVID-19 vaccination requirement for workers at adult-care facilities, jails and prisons. Individual businesses or other institutions can still continue vaccination requirements.
Most healthcare workers are required to be vaccinated against COVID-19. The federal rules apply to healthcare facilities that accept money from Medicare and Medicaid.
Also on Monday, California will lift its order for everyone to mask up in healthcare settings.
L.A. County isnât going that far. Officials will lift a mask order for visitors and patients at healthcare settings, but retain the requirement for healthcare workers providing patient care or working in patient areas.
âEverything we know right now says that these masks provide protection. And we really donât have lots of healthcare providers saying they donât think they need to be wearing these masks,â Ferrer said. The possibility an infected doctor or nurse could transmit the coronavirus to a vulnerable patient could âresult in a devastating and severe illness.â
A new study examines the factors that caused some states to have COVID-19 mortality rates that were four times higher than others.
The pivot from conflict to coexistence with COVID-19 is reflected in the steady unwinding of emergency rules and declarations put in place during the pandemicâs early onslaught.
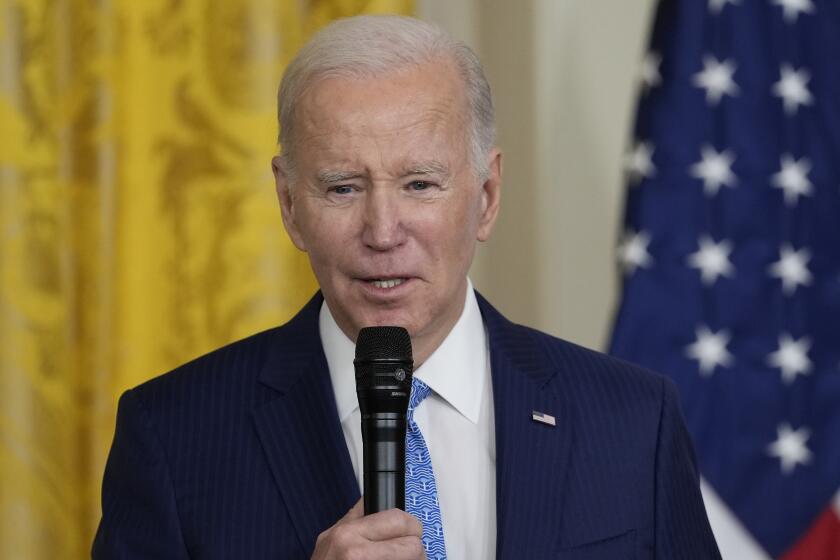
Gov. Gavin Newsom formally rescinded Californiaâs three-year-old statewide emergency declaration at the end of February. President Biden previously informed Congress he would rescind the national-level emergency and public health emergency declarations May 11, though congressional Republicans are pushing to do so earlier.
Springâs arrival has ushered in rosy conditions across California â with all 58 counties recording transmission and hospitalization rates in the low community level.
That category, defined by the U.S. Centers for Disease Control and Prevention, indicates that the coronavirus is not spreading at a rapid pace or in a way thatâs exerting undue stress on the healthcare system.
L.A. Countyâs coronavirus case count is the lowest itâs been since July 2021, shortly after the first wave of widespread vaccinations but before the arrival of the Delta variant. For the seven-day period that ended Tuesday, the county reported an average of 501 cases a day, or 35 cases a week for every 100,000 residents.
President Biden wonât veto a Republican-led measure to end the national COVID emergency, despite having expressed strong objections against it earlier this year.
COVID-19 continues to exact a deadly toll. For the seven-day period that ended Tuesday, 58 L.A. County residents with a coronavirus infection died. Thatâs lower than the winter peak of 164 in early January, but still higher than last autumnâs lull of 43, and last springâs low of 24.
Cumulatively, nearly 36,000 coronavirus-infected people have died in L.A. County. More than 101,000 COVID-19 deaths have been reported across California; nationwide, the death toll is 1.1 million.
And while the toll was lower this winter, COVID-19 was still a significant cause of death. Nationally, 69,000 COVID-19 deaths were reported since October, nearly quadruple the estimated 18,000 flu deaths over the same period.
People at highest risk of dying remain the unvaccinated, including those who have been infected before. For the 30-day period ending Feb. 14, unvaccinated Angelenos were more than six times as likely to die from COVID-19 compared with those who were vaccinated and had received an updated booster shot.
And long COVID continues to be a risk. One survey suggested that about 1 in 4 adults nationwide who had COVID-19 contend with long COVID symptoms lasting three months or longer. Most people with long COVID slowly improve, but the illness of some persists for years, resulting in disability, Ferrer said.
Itâs 2023 and you just tested positive for COVID-19. Now what? The latest CDC protocols, isolation recommendations, ways to treat it and ways to prevent long COVID.
L.A. County has seen a steady and sustained slide in its pandemic-related hospital census in recent months. Since early December, when healthcare systems were still contending with the fallout from a fleeting autumn spike, the number of coronavirus-positive patients has tumbled from more than 1,300 to just below 400 as of Wednesday.
That count, which includes those hospitalized specifically for COVID-related illness and those who incidentally test positive after seeking care for another reason, is the most meager single-day tally since October. But it remains above the previous lows in the spring of 2021 and 2022, when hospitalizations fell to 212 and 209, respectively.
Though the emergency phase of the pandemic is swiftly coming to an end, officials warn the danger is not yet over. One particular concern, Van Kerkhove said during a briefing Wednesday, âis the potential for the virus to change, to become not only more transmissible but more severe.â
âWe will continue to see waves of infection,â she said. âThe peaks of those infections may not be as large as we saw before, and likely will not be because we have population-level immunity that has increased around the world from vaccination and also from past infection.â
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.