Why Californiaâs much-touted CARE Court is âno one-and-done programâ
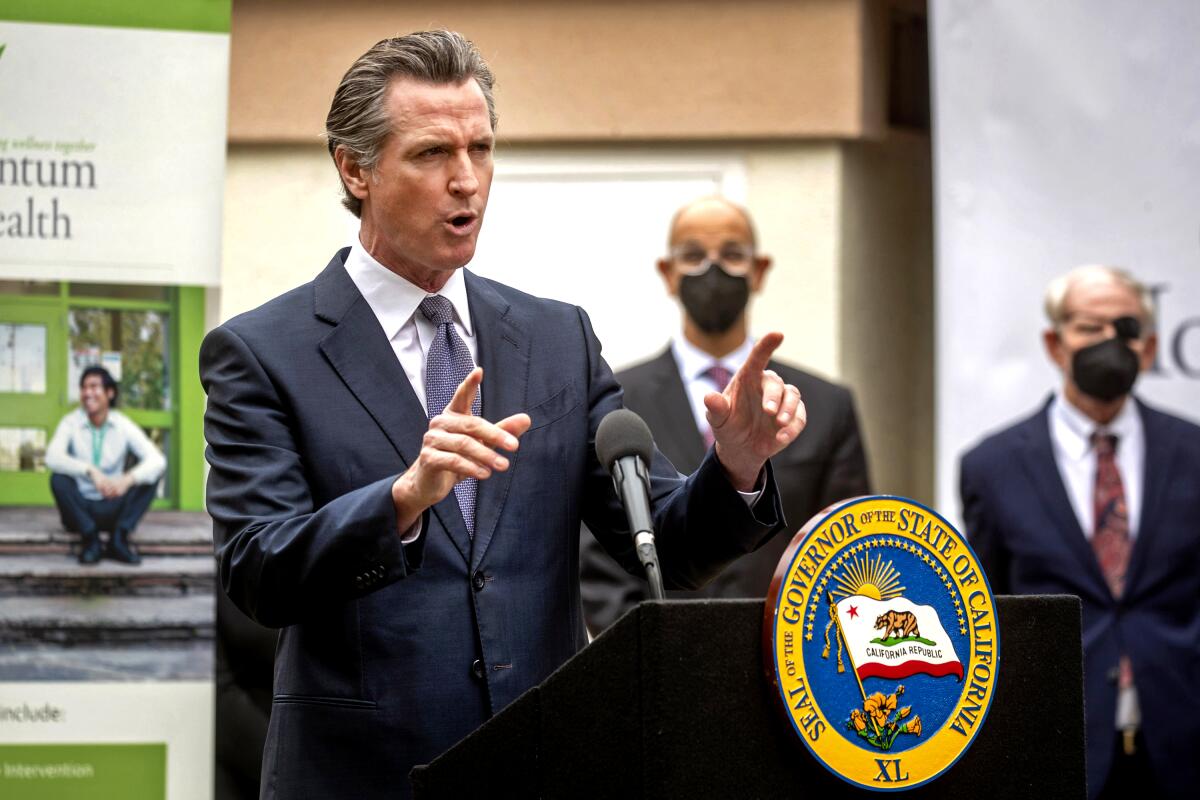
When Gov. Gavin Newsom signed the CARE Act into law in September, he set the clock on seven counties to have the program with its signature courts up and running by Oct. 1, 2023.
The graduated rollout gives the rest of the state, including Los Angeles County, until December 2024, but the Community Assistance, Recovery and Empowerment Act has already been hailed as a fix for the stateâs broken behavioral health system, a road to recovery for those who are severely mentally ill.
Three months into implementing its provisions, however, mental health directors advise against setting expectations too high. They point to the logistical and financial challenges of launching a labor-intensive program from scratch, as well as the limiting effect of a decades-old law already on the books governing the treatment of mentally ill people in California.
âThe language attending the rollout of this has been heady and leaned into phrases like âtransformative,â â said Luke Bergmann, director of behavioral health services for San Diego County, which is working to meet the deadline. âBut the changes will likely be incremental.â
Veronica Kelley, behavioral health director for Orange County, which has also been tagged for the early rollout, has been working with the National Alliance on Mental Illness âto make clear what CARE Court is and what it isnât.â
âThere is no involuntary medicatingâ of people, she said. âThis isnât a housing program. This is no one-and-done program.â
Though the tragedy playing out among those living with severe mental illness in homeless encampments throughout the state frequently elicits calls for immediate and declarative action, the complexity of the issue defies a quick fix â by intent.
In L.A. County, CARE Court will be implemented next year. Hereâs how you can access it.
The stateâs history of incarcerating mentally ill people in asylums through the 1960s still casts a long shadow from when it institutionalized up to 37,000 people in the mid-1950s, many of them indigent, vagrant â the âhyper-marginalized,â as Alex Barnard, assistant professor of sociology at New York University, has described them.
Despite sweeping claims, the CARE Act â like other attempts to legislate treatment for severe mental illness â is constrained by the Lanterman-Petris-Short Act, which was passed in 1967 as the state began closing down many of its state mental facilities after decades of neglect and abuse of patients.
LPS â as it is known â defined how far the state can go toward forcing someone to be hospitalized and to take psychiatric medication. In an attempt to balance the need for treatment and respect for autonomy, it established criteria for conservatorship either by a family member or a public guardian.
âThe LPS Act was landmark legislation recognizing the complex intersection of mental illness and civil rights. It remains for the most part a widely accepted, precedent-breaking set of regulations,â said Rod Shaner, who served as medical director for the Los Angeles County Department of Mental Health from 1996 to 2018.
Any attempt âto undermine its core foundation would likely be unsuccessful,â Shaner said. âA wiser and more practical course would be to carefully re-sculpt limited areas and not bring in a new block of marble.â

Today, LPSâ legacy is mixed. For some, it is a singular impediment. In 2020, then-state Sen. John Moorlach (R-Costa Mesa) introduced a bill to repeal and replace LPS. It died in committee.
For others, LPS is a necessary safeguard against locking up people without due process.
Disability Rights California, which opposes the CARE Act, argues that the legislation âis based on stigma and stereotypes of people living with mental health disabilities and experiencing homelessness and will disproportionately impact Black Californians ⌠furthering institutional racism.â
âThere is a crisis, but what the Legislature often does is apply Band-Aids to problems â as opposed to coming up with a big-picture solution â because that is either too difficult or there isnât enough time or will,â said Deb Roth, a senior legislative advocate for the organization.
How successfully the CARE Act straddles these lines, experts say, will depend on both its implementation in the coming months and its interpretation once the courts open.
How the CARE Act works
As mental health agencies struggle to contain a crisis where homelessness is often the common fate for those with severe mental illness, the CARE Act was written as an attempt to increase pressure on those who might resist treatment, described by Newsom in his announcement as âpeople with the hardest-to-treat behavioral conditions.â
With 10 months to put all the pieces in place, Bergmann and Kelley have been meeting with behavioral health directors of the other five early counties â Glenn, Riverside, Stanislaus, Tuolumne and San Francisco â to help one another implement the law and meet its obligations by the October deadline.
The logistics themselves are straightforward.
Prior to the CARE Act, only trained professionals could petition a court to order county intervention for an individual with psychosis, but now a far wider range of petitioners â notably families, domestic partners, roommates â can appeal to the court.
Once a petition has been received, a judge will direct an assessment team to conduct interviews and determine if criteria specified by the law, namely untreated schizophrenia or related psychotic disorders, are met. The team will then put together a treatment plan and seek voluntary compliance.
Failing that, a hearing will be called, and the judge, working with the individual and a public defender, will make the necessary orders, review and update treatment and assess progress. The treatment plan can be ordered for 12 months and, if necessary, renewed for another year.
For Bergmann, one of the challenges is related to budgeting, hiring and training. The California Health and Human Services Agency estimates that between 7,000 and 12,000 people may meet the CARE criteria, but âit is hard to anticipate how many petitioners there will be â and how to scale the necessary infrastructure,â he said. âWeâre already shorthanded.â
Like other counties in the state, San Diego County is facing an acute shortage of mental health workers. The county anticipates needing up to 18,000 more workers if it is to keep up with demand.
Kelley said the courtroom structure of the CARE Act will borrow from what already exists in collaborative justice courts, where judges work with behavioral health officials and public defenders to come up with treatment options rather than jail time for offenders whose crimes were committed on account of mental illness or addiction.
In addition, she said, âwe also have AOTâ as a logistical model for CARE Court.
AOT, or assisted outpatient treatment, is the signature program to come out of the 2002 Lauraâs Law. It also requires individuals, who meet specific criteria for their mental illness, to stand before a judge who oversees a treatment plan. Because it too is constrained by the same LPS detention and treatment limitations, it is a good example of what the CARE Act can and canât accomplish.
Lauraâs Law faces its own hurdles
When Scott Harlan Thorpe killed three people and wounded two in a Sierra Nevada town northeast of Sacramento in January 2001, the tragedy highlighted for some the shortcomings of the LPS Act. The law had no provisions for treating those with severe mental illness who did not meet the established criteria for involuntary detention or public guardianship.
Those criteria established that individuals who were a danger to themselves or others or âgravely disabledâ â unable to provide for the basic needs of food, clothing and shelter â could be forcibly detained for a specific time depending on their response to treatment.
Thorpeâs condition lay outside those criteria. As much as his family tried to get him help for his deepening paranoia â he thought the FBI was trying to poison him â he refused.
Concerned that LPS went too far toward respecting the autonomy of mentally ill people over their need for care, legislators began drafting Lauraâs Law, named for one of the victims.
Their goal was to establish a court-ordered treatment program for individuals whose illness had led to a hospitalization or incarceration or had resulted in violent behavior. AOT would provide psychiatric care outside a mental health facility through outpatient conservatorship.
But AOT, signed into law in 2002, did not fully realize the lawmakersâ original intent, Shaner said.
First, rather than being a sweeping reform, the legislation allowed each county in the state to decide if and when to implement AOT. Many, citing a lack of funding, held off; Los Angeles waited until 2014. (Not until two years ago were counties required by new legislation either to participate or to opt out. As of last year, a little more than half of the state had adopted AOT.)
Second, patients could not be ordered to comply with a treatment plan. Instead, AOT relied on what is known as âthe black robe effect,â the presumption that standing in the presence of a judge is enough to compel adherence to a plan.
Otherwise, the most recalcitrant could be held for 72 hours while being assessed for a longer hold, and if they didnât meet LPS criteria, they would be released to the street without additional help.
âAOT didnât change the basic LPS detention criteria one iota,â Shaner said, evidence of LPSâ continuing reach.
The CARE Act faces similar limitations.
The life of a 31-year-old living with schizophrenia illustrates the toll of illness and the challenge of getting severely mentally ill people off the streets.
Though a judge may order the care and treatment plan for someone with schizophrenia or a related psychotic disorder, that individual cannot be forced into treatment or forcibly medicated unless they are subject to constraints defined by the LPS Act, according to a spokesperson for the California Health and Human Services Agency.
Perhaps that is fine, said Barnard, at New York University. âThe theory behind AOT and CARE Court is that not everyone needs to be hospitalized. Maybe they just need an incentive â even if it is coercive, coming from a judge,â he said, citing the black-robe effect.
Even then, the effectiveness of such treatment programs â involuntary, outpatient, even when overseen by a judge â is being questioned. A recent UCLA study raised doubts about the effectiveness of AOT due to âinadequate resources, inadequate continuity of care and client attrition.â
Roth, with Disability Rights California, has similar reservations about the CARE Act. âIf you look at what they are doing with CARE Court,â she said, âit is unclear that there will be the resources that they say are needed to help people.â
She is also troubled that the prospect of bringing individuals with severe mental illness into a courtroom setting will introduce trauma into their lives and exacerbate their condition. âThese are people who probably already have experienced trauma whether they have serious mental illness or not,â she said.
Despite these concerns, behavioral health directors Bergmann and Kelley see the CARE Act as a tool, like LPS and AOT, for trying to help those with the worst symptoms of mental illness.
Bergmann, though, is under no illusions that this is all thatâs needed.
âI worry about the logistical challenges,â he said, âbut what keeps me up at night are the larger challenges we face meeting the needs of people for many years into the future. Whatever success Care Court has, it wonât look good if we donât figure out how to increase long-term care â and that includes residential placements.â
Meanwhile, lawmakers in Sacramento are looking at ways to modify LPS so it better addresses the reality of mental illness and homelessness in the 21st century.
Since 2018, Assemblymember Miguel Santiago (D-Los Angeles) has introduced a series of bills that would have expanded LPSâ definition of grave disability to include the inability to seek treatment for serious medical conditions. None of them passed.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.














