How much worse will coronavirus crisis get in L.A. County? Here is what next few weeks could look like

- Share via
How bad will the next few weeks get?
The number of COVID-19 deaths in California and Los Angeles County — an epicenter of the pandemic — is setting records or near-records almost daily. There is clear evidence that the post-Christmas holiday surge in cases is worsening, as the numbers continue to spike, particularly in L.A. County.
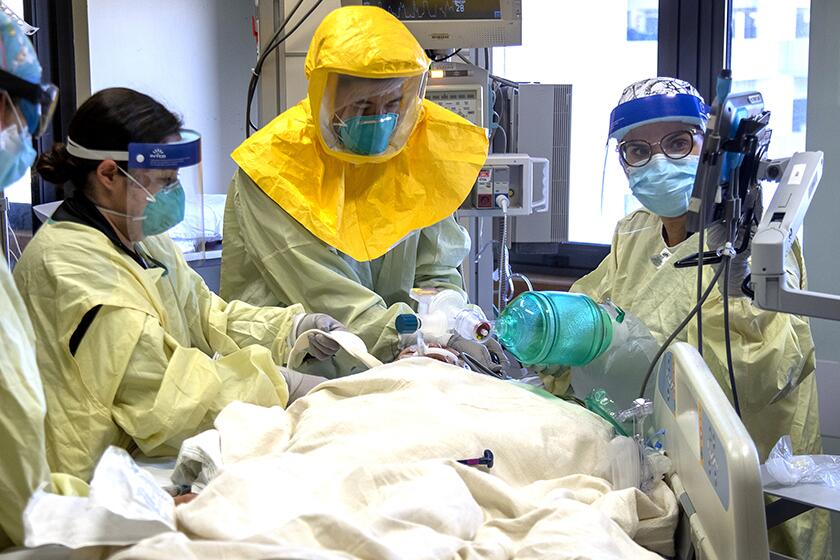
But the big question is whether this new wave of cases will result in a similar increase in hospitalizations as occurred during the post-Thanksgiving surge, which has pushed hospitals to the breaking point, resulting in terrifying shortages of staffing and certain supplies and affecting the quality of medical care given to critically ill patients.
Around Thanksgiving, about 300 new COVID-19 patients a day were admitted into hospitals in L.A. County; that number rose precipitously for about a month, finally stabilizing at about 750 to 800 new hospitalizations a day around Christmas Eve. Another doubling or tripling of new hospitalizations per day would be catastrophic.
For as dire as the crisis has become, most hospitals have yet to enter a sustained, widespread period of rationed care. But that would probably come if the Christmas surge is dramatically worse.
Teams of triage officers — usually led by critical care and emergency doctors — would have to be fully activated. Faced with shortages in staff and supplies, they would be forced to make the most heart-wrenching decisions: determining who receives the most aggressive lifesaving care and the limited time of the best-trained professionals and equipment, and who is given a lesser chance of survival and provided treatment to comfort them as they die. How hospitalizations break this week will give officials a sense of what to expect.
“We are all waiting with a certain amount of anxiety in seeing how the hospital admission data unfold over the coming days,” said Dr. Roger Lewis, director of COVID-19 hospital demand modeling for the L.A. County Department of Health Services.
“The hospital-based system is literally at the breaking point, where a substantial increase in demand could result in situations where we cannot provide to people the care that we would all expect to be able to provide or to receive when we’re critically ill,” he added.
Researchers share which numbers they’re watching to forecast when California’s deadly COVID-19 surge will end.
Patients suffering from COVID-19 who are now entering the hospitals were mostly infected in the post-Thanksgiving, pre-Christmas period. The flattening of new hospitalizations probably resulted from the imposition of stay-at-home orders issued by the county and state.
But the effect of holiday gatherings over Christmas will soon begin to show up in hospitals. Soon, a certain percentage of people who got infected over Christmas and have tested positive will begin getting so sick they’ll need hospital care. If the number of new daily hospital admissions for COVID-19 patients worsens, that’s a big sign of trouble.
Now, it’s possible that the increasing hospitalizations could be moderated if, for instance, it’s mostly younger, otherwise healthier people who got infected over the holiday season, and quarantined or isolated themselves to avoid infecting older family and friends who are at a higher risk of dying.
But it’s also plausible the vulnerable and elderly people attended Christmas and New Year’s gatherings or were later infected by younger people who didn’t stay away from them — something that happened over the Thanksgiving holiday.
“The fear, or the intuition, of most of the people doing predictive modeling is that it is going to get worse. The uncertainty is in how much worse. And in order to quantify how much worse, that requires the data that will only be available to us next week,” Lewis said.
After a sale to UCLA, Olympia Medical Center says it will shut down March 31. Workers and community members said they were blindsided by the decision.
The post-Christmas surge in new coronavirus cases has been growing by the day. L.A. County’s average number of new coronavirus cases on Thursday, Friday and Saturday was about 18,000 — significantly above the average of about 14,000 new cases a day over the last week.
“This very clearly is the latest surge from the winter holidays and New Year’s — no question about it,” said the L.A. County Department of Public Health’s chief science officer, Dr. Paul Simon. “It had gradually started earlier in the week, but [definitely] here in the last day or two.”
About 1 in 5 coronavirus tests performed daily in Los Angeles County are coming back positive, a huge increase from early November when about 1 in 25 tests confirmed an infection. And when community transmission is this prolific, officials warn that activities that seemed mundane months ago carry a higher risk of infection than ever.
Simon said the increase in daily coronavirus cases is likely to continue over the next week or two, which will translate into even worse hospitalizations and more deaths. The number of daily COVID-19 deaths is already breaking records; in early December, about 30 people a day in L.A. County were dying of COVID-19 on average over a seven-day period; now, about 200 people a day are dying.
The number of people dying of COVID-19 daily is now exceeding the average number of deaths in L.A. County for all other causes, including heart disease, cancer, stroke, diabetes, car crashes, suicides and homicides, which is about 170 deaths a day.
EMTs are waiting four, five and even 10 hours to offload patients at hospitals, officials said.
Some veteran epidemiologists suspect higher levels of hospitalizations and deaths will, in fact, materialize and that hospitals will be forced to adopt “crisis standards of care,” in which triage doctors may have to choose who receives lifesaving treatment.
“I anticipate that with the increased numbers of cases that we are seeing — which will translate into inevitable increased numbers of hospitalizations and ICU patients — that hospitals will be forced into operating under crisis protocols that may include rationing of care,” said UCLA medical epidemiologist and infectious-diseases expert Dr. Robert Kim-Farley.
Kim-Farley said he suspected there will be a renewed increase in hospitalizations soon that will continue rising through the end of January. A fraction of those people won’t survive their illness, and a peak in daily COVID-19 deaths will probably occur in mid-February, Kim-Farley said, due to the lag between initial hospitalization and death.
It was wise that state officials are ready to distribute dozens of large refrigerated trailers that can act as temporary morgues for bodies that are being dispatched to counties, Kim-Farley said. Funeral homes across the state are already overwhelmed by the surge in bodies and some have been forced to turn families away.
“Unfortunately, the surge capacity being done for morgues will in fact be needed,” Kim-Farley said.
L.A. County has now reached new milestones in the pandemic: more than 12,000 dead from COVID-19 and more than 900,000 coronavirus cases.
On Saturday, 218 COVID-19 deaths were reported in L.A. County. That came the day after the county set a single-day record of 318.
L.A. County officials Saturday confirmed three additional cases of the coronavirus-related inflammatory disease in children known as MIS-C. A total of 54 children in L.A. County have contracted the severe illness, and one has died. The disease can cause fever and inflame the heart, lungs, kidneys, brain, skin, eyes and gastrointestinal organs. The disease is disproportionately affecting Latino children, who account for about 3 of 4 reported cases.
In L.A. County in recent days, available ICU beds fell to zero or one in each of the following regions: central L.A., the Westside, southeast L.A. County, the San Gabriel Valley and the Antelope Valley. The South Bay-and-Long Beach region had as few as three available ICU beds in recent days, and the San Fernando Valley as few as six.
In Santa Clara County, which has some 2 million residents, about 20 to 25 available ICU beds remained Friday; in Fresno County, with about 1 million residents, only 10 beds were available.
Dr. Rais Vohra, Fresno County’s interim health officer, said hospitals are preparing for “a very hard rest of January and possibly February,” including scrambling to find supplies related to providing oxygen treatments and providing ways to perform infusions of antibodies to keep patients from needing hospitalization.
Some help has started to arrive: Staffers from the U.S. Department of Defense, as well as ICU nurses recruited by the state, have been deployed around hospitals in the region, said Dan Lynch, director of the Fresno County Emergency Medical Services agency. And one hospital in San Mateo County has offered to take in critically ill patients from Fresno County.
But it won’t be easy to do those transfers in practice. “It is a risky move when you’re moving them for a long distance,” Lynch said.
Though California’s existing pandemic surge is dire, the state has one of the lower cumulative numbers of COVID-19 deaths on a per capita basis, ranking 38th among the 50 states, probably a result of the early imposition of the stay-at-home order in the spring and summertime closures of certain high-risk businesses. New Jersey’s cumulative COVID-19 death rate is triple that of California’s; Arizona’s is double.
Times staff writer Ryan Murphy contributed to this report.
More to Read
Sign up for Essential California
The most important California stories and recommendations in your inbox every morning.
You may occasionally receive promotional content from the Los Angeles Times.