Price of a common surgery varies from $39,000 to $237,000 in L.A.

U.S. hospitals charged Medicare $54,239, on average, for joint-replacement surgeries in 2013. That was up 3.8% from the previous year.
A short drive in the Los Angeles area can yield big differences in price for knee or hip replacement surgery.
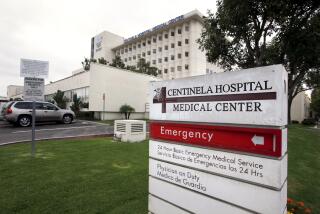
New Medicare data show that Inglewoodâs Centinela Hospital Medical Center billed the federal program $237,063, on average, for joint replacement surgery in 2013.
That was the highest charge nationwide. And itâs six times what Kaiser Permanente billed Medicare eight miles away at its West L.A. hospital. Kaiser billed $39,059, on average, and Medicare paid $12,457.
The federal program also paid a fraction of Centinelaâs bill -- an average of $17,609 for these procedures.
The average charge nationwide for a major joint replacement operation was $54,239, according to federal figures.
Joint replacement surgeries are Medicareâs most common inpatient procedure, costing the federal government more than $6.6 billion in 2013.
Overall, the latest data show what hospitals charged and what Medicare paid for 100 of the most common inpatient stays and the 30 most common outpatient procedures. The inpatient data cover more than $62 billion of Medicare money.
The Obama administration first released this type of data two years ago to put heat on hospitals to explain wildly different charges for the same treatment at medical centers across the nation.
Both government officials and employers are demanding more pricing transparency to spur greater competition in hopes that it can help control ever-rising medical costs.
Monday, Medicare also published its second annual set of physician payment data.
The highest-paid specialists nationwide were radiation oncologists, who received an average of $403,512 in Medicare payments. Next were dermatologists at $331,108 and then vascular surgeons at $329,874.
Medicare âwill continue to release the hospital and physician data on an annual basis so we can enable smarter decision making about care that is delivered in the healthcare system,â said Niall Brennan, chief data officer at the Centers for Medicare and Medicaid Services.
Hospitals often say billed charges are irrelevant because they donât reflect what Medicare or health insurers actually pay. But these charges can influence the ultimate cost for employers and consumers.
Health insurance companies tie some reimbursements to these list prices. Consumers going out of their insurance network or cash-paying patients can face these higher charges.
A spokeswoman for Prime Healthcare Services, which owns Centinela Hospital, said costs should be evaluated based on reimbursements, not billed charges since those are âmisleading, confusing and in many cases inaccurate.â
Prime said the new government data show that the Centinela hospital received lower reimbursement from Medicare than a third of the 242 California hospitals listed.
Other area hospitals also sported higher-than-average charges.
Cedars-Sinai Medical Center billed Medicare $123,684, on average, for joint replacement surgeries and got paid $15,650.
UC Irvine Medical Center charged less, $104,141, but got reimbursed more -- $20,604.
The data released this week exclude the privately run Medicare Advantage plans as well as payments for Part D prescription drug plans. That pharmacy data was published earlier this year.
Twitter: @chadterhune
More to Read
Inside the business of entertainment
The Wide Shot brings you news, analysis and insights on everything from streaming wars to production â and what it all means for the future.
You may occasionally receive promotional content from the Los Angeles Times.