Patients pay a higher share of hospital bills, study finds
Patients, even those with employer-sponsored health plans, may face another condition after they are discharged from a hospital stay: acute sticker shock.
Out-of-pocket hospitalization costs rose 37% from 2009 to 2013, with the average patient paying more than $1,000 per hospital visit, according to a study conducted by the University of Michigan. The survey took place before many of the Obamacare provisions were in place, including the health insurance marketplaces.
Driven by an 86% rise in deductibles and a 33% increase in coinsurance â the part of the hospital bill that patients are expected to pay â the out-of-pocket costs rose faster than health insurance premiums.
The higher cost-sharing burden may surprise some patients, particularly those with employer-sponsored plans, according to Emily Adrion, a University of Michigan research fellow and lead author of the study published Monday in the journal JAMA Internal Medicine.
âPeople tend to assume theyâre fine, theyâll be covered and will not be responsible for any sort of high cost when theyâre hospitalized,â Adrion said Monday. âMost people expected they wouldnât have to pay much if they were hospitalized.â
The study looked at 7.3 million hospital stays from 2009 to 2013, using data from Aetna, UnitedHealthcare and Humana insurance companies. It found that out-of-pocket spending climbed at a 6.5% annual rate. At the same time, health insurance premiums rose 5.1% annually, while the annual growth in healthcare spending was slower, at 2.9%.
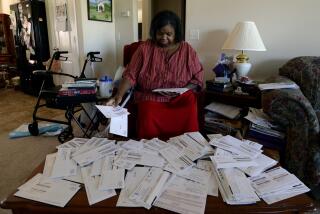
Adrion said the data show that employers were shifting more costs to the patients. She said the complexity of most health insurance policies means that many patients donât know how much more they are responsible for paying â until they are discharged from the hospital.
âWith really high out-of-pocket costs â particularly in the form of coinsurance â that can be really surprising and unexpected,â Adrion said. âPeople end up going to a hospital and not knowing what considerable financial risk they are facing.â
About 85% of health insurance benefit packages required coinsurance for inpatient hospitalizations, in addition to meeting an annual deductible, the study said.
For those with consumer-directed plans â high deductible policies paired with health savings accounts â out-of-pocket hospital costs topped $1,200, while patients with individual plans paid more than $1,800 on average, the study showed.