U.S.-Thai Trial for AIDS Vaccine Slated
BARCELONA, Spain — The U.S. and Thai governments will shortly begin the largest trial yet of a preventive AIDS vaccine, testing a combination of vaccines on more than 16,000 subjects in the general Thai population, researchers from the two countries announced here Monday at the 14th International AIDS Conference.
The trial, originally sponsored in a slightly different form by the Defense Department, was canceled in February. After a small reconfiguration to change its goals, the $36-million effort will now be funded by the National Institute of Allergy and Infectious Diseases, which has taken over the AIDS programs formerly operated by the military.
There has been much debate over when new candidates should be tested and what criteria should be used, said NIAID director Dr. Anthony Fauci. “But at the end of the day, we have to have candidates in trials. Even if they fail, we will learn things that are very important.”
In another development, Brisbane, Calif., biotechnology company VaxGen Inc. said a commercial AIDS vaccine could be available by 2005 if two major trials now nearing completion are successful.
Although data from VaxGen’s trials of 7,900 subjects will not be available until early 2003, experts said the mere fact that the trials were successfully carried out represents a substantial step forward in the quest to control the AIDS virus, which is expected to have infected 110 million people by 2020.
Critics had argued that it would not be possible to complete the study because of the difficulties involved in monitoring large numbers of high-risk patients for three years or longer.
“Just the fact that they pulled this off is reason for optimism,” said Dr. Carl Dieffenbach of the NIAID.
Nonetheless, critics cautioned that AIDS vaccines have offered high promises in the past.
Researchers have been searching for an AIDS vaccine since the syndrome was first recognized 21 years ago. “An effective vaccine is our only hope of stemming the epidemic,” said Sandra L. Thurman, president of the International AIDS Trust.
More than 30 candidate vaccines have already been put through phase 1 and phase 2 clinical trials, designed to test safety and determine whether the candidates have any effect. Eight are currently undergoing such trials.
The VaxGen product, called AIDSVax, was the first to enter phase 3 trials, the final large trials required before a new drug or vaccine can be approved by a regulatory agency.
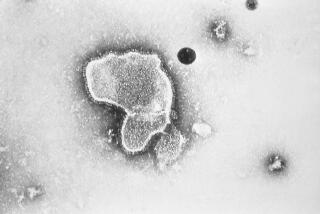
AIDSVax is a classic vaccine very much like those used to control polio, measles and a host of other infectious diseases. Viral surface proteins produced by genetic engineering techniques are administered to stimulate production of antibodies that will attack viruses before they can invade cells.
“Antibodies protect against viral infection, we know that,” said Dr. Donald P. Francis, president of VaxGen. “Everyone who gets the vaccine develops an immune response. The question is, does it last long enough and provide protection?”
VaxGen is sponsoring two trials, one in North America and the Netherlands involving 5,400 people who are at risk of contracting the virus through sexual transmission, and one in Thailand involving 2,500 intravenous drug abusers. In each group, half receive the vaccine and half a placebo. The three-year project has involved 1,000 workers, 127,408 blood samples and about 1.3 million paper forms, Francis said--enough to form a stack “30 feet taller than the Statue of Liberty.”
Francis said that, despite rumors, VaxGen had received absolutely no hints about the potential results of the trials. He called the rumors “hogwash.”
What they do know, he added, is that the safety data monitoring board, which oversees the trials, has said that there are sufficient numbers of infections in the placebo group to indicate that the trials will provide a result.
No one expects the vaccine to be 100% successful. But extensive modeling studies have indicated that even a 30% efficacy rate would be enough “to drive the epidemic into the ground,” Francis said.
“A little bit of immunity goes a long way,” said the NIAID’s Dieffenbach.
“If we get a 30% efficacy, I’ll be thrilled,” Francis said. “Once we have some efficacy, we can always increase it.”
Francis noted that the company has already begun building a manufacturing facility in anticipation that the trials will prove the vaccine works.
The alternative approach to AIDS vaccine development--one that many experts hold higher hopes for--aims to stimulate the production of white blood cells called cytotoxic lymphocytes that attack and destroy cells already infected by the virus.
The NIAID’s Thai test will use such a vaccine, developed by the French company Aventis Pasteur and called Alvac-HIV, followed by administration of AIDSVax. This approach is called “prime-boost” because the immune system is primed with the first vaccine, then boosted with the second. That test will be the second phase 3 trial to take place.
Alvac-HIV is a live-virus vaccine based on the canary pox virus, which has previously been used in veterinary vaccines and does not infect humans. Aventis Pasteur researchers have engineered the virus so that it contains the genes for several proteins that are normally part of HIV.
The canary pox vaccine has been tested in humans for more than six years and has been shown to be completely safe, NIAID director Fauci said. Those tests have suggested that it provides protection, but that can be determined only in a much larger trial.
The original Defense Department-sponsored trial that was canceled in February was designed to determine what researchers call “correlates of immunity”--that is, what changes in the immune system indicate that vaccination produces protection. But an analysis of the proposed trial indicated that, as designed, it could not yield that information.
With slight changes, however, it can determine whether the vaccine works, he said. “This is an efficacy trial, with those other things only secondary.”
The trial is being conducted in Thailand, which has a long history of work on an AIDS vaccine, because the prevalence of the disease there means meaningful results can be obtained relatively quickly.
“We don’t know what the outcome will be,” said Dr. Vallop Thaineau of the Thai Ministry of Public Health.
“But we know for sure that we will learn a lot.”